Ifeoma Okoye is a Professor of Radiology, College of Medicine, University of Nigeria, Nsukka/University of Nigeria Teaching Hospital Enugu (UNTH), Enugu State. She is also the Director, University of Nigeria Centre for Clinical Trials (UNNCECT), and Founder /Co-Chair African Clinical Trial Consortium. Okoye, who is also the founder, Breast Without Spot (BWS), a non-governmental organisation (NGO), in this interview with CHUKWUMA MUANYA explains why Nigeria has one of the highest cancer cases and deaths globally. She, however, made recommendations on how to reduce the rising cancer cases and deaths in the country.
Why are we recording more cancer cases and deaths globally?
Predictably, the situation is getting worse. In the past years, the government showed some commitment in making more cancer screening and treatment facilities available. However, the unprecedented pandemic has resulted in, perhaps diversion of funds (not substantiated by any evidence), and other available resources, to COVID-19 screening and treatment.
In the first wave, some hospitals such as Asokoro District Hospital were dedicated solely to isolation and treatment of COVID-19 patients.
Additionally, some hospital oncology practices had to take a chance in triaging their cancer patients to reduce the risk of them being exposed to COVID-19, if allowed to still make their regular routine visits required for follow up with either their chemotherapy or radiotherapy management. Those patients needing surgical interventions were shelved for a while, as hospitals battled to familiarise themselves with creating a balance between exposing HealthCare Workers (HCWs) to unidentifiable cancer patient with the double jeopardy of having COVID-19.
Thus, hospital theaters were shutdown, except for emergencies, even that with a lot of apprehension, as the test kits used in those earlier months were not the fast Polymerase Chain Reaction (PCR) testing services. Thus, even emergencies had to cool their heels to await verification of their status. This protocol mostly prevailed, unless in hospital facilities where the HCWs had a death wish or chose to stand with the conspiracy theory that there was no COVID-19.
What is the latest statistics on cancer cases, deaths and morbidity in Nigeria?
Cancer is a leading cause of morbidity and mortality globally and has become a disease of public health concern. The global distribution of predominant cancers has continued to change especially in developing countries. While the low and middle-income countries accounted for 51 per cent of all cancers worldwide in 1975, the proportion increased to 55 per cent in 2007 and to 70 per cent in 2018. It is necessary for all hands to be on deck to put an end to this ugly trend.
Data from the Cancer Registries across the country as reported by the Nigeria National System of Cancer Registries (NSCR) has been very useful in the formulation of evidence-based cancer control policies and programmes. The activities of NSCR have improved cancer research in Nigeria and have been a reliable source of epidemiological data from Nigeria to Globacan, the global Cancer research agency.
Cancer in Nigeria 2009-2016, which is the second edition of the publications of NSCR, provides cancer data from 18 Cancer Registries across the country including the National Cancer incidence, which was derived from six population-based Cancer Registries nationwide (Abuja, Calabar, Edo, Enugu, Ekiti and Sokoto). It also provides information on the incidence of cancers from different regions of the country, as well as the commonest cancers in Nigeria both by sites and by sex. This book also provides detailed history of cancer registration in the nation including the successes and the challenges associated with cancer registration and possible ways of mitigating them.
We are yet to collect recent data; we are still officially using the data as at 2018, which was the Globocan projection from 2013/2014 publication (source for above view is from Hon Minister of Health, speech at 2020, International Cancer Week, in October @ Abuja)
Can cancer be avoided or rather prevented?
It may not be possible to completely avoid cancer, but there is a lot we can do to reduce the risk of getting some cancers and detecting them early through routine screening. And for cervical cancer, fortunately, there is available and accessible efficacious vaccination (HPV: Human Papilloma Virus, Vaccine) that easily achieves primary prevention!
To improve early detection, we need to put the following in place: community advocacy/mobilisation (planned and annually rostered and sustained; and awareness campaigns. More effort should be focused on screening programmes, and imperatively, the often forgotten need of providing training/capacity building of health workers, particularly, community health workers and nurses who serve as primary contacts for women in rural areas.
What are your recommendations on how best to stop cancer?
Our strong recommendation is for a shift of focus from ‘sick-care’, to ‘preventive care’, with attention to lifestyle modifications and control of environmental pollutants /food additives/sharp practices in food production and manufacture and gating of the window period between our farms and the market places that distribute food to the consumers (end users of food products)
What are these, environmental pollutants/food additives/sharp practices in food production and manufacture?
Poor handling of refuse disposal, such that both biodegradable and non bio-degradable are left to cause a lot of putrefaction fumes, and release of dangerous bio-wastes that can pollute also our drinking water sources, available to both humans and livestock!
Vehicular fumes and industrial fumes contribute seriously to environmental air pollution in Nigeria. Last year, the World Bank reported that 94 per cent of the population in Nigeria is exposed to air pollution levels that exceed WHO guidelines (compared to 72 per cent on average in Sub-Saharan Africa in general) and air pollution damage costs about one per cent post of Gross National Income (2015)! Environmental pollution contributes up to 80 per cent to risk factors for cancer! Some mining areas like Jos, they mine tin, lead and iron ore; coal in Enugu and so on. These are all emitters that have implicated carcinogenic effects, often by direct exposure or contaminants of drinking water.
Food additives/sharp practices in food production and manufacture and handling! Examples are ripening agents like carbide used by sellers of fruits to ripen fruits such as banana, pawpaw, mangoes, etc. Food colouring to redden stews, palm oil, food enhancers with bleaching and carcinogenic properties, containing MSG (monosodium Glutamate), cubed and powdered enhancers, sweeteners with Aspartame, uncontrolled use of insecticides/pesticides to de-weevil grains and antibiotics, hormones in poultry and fish farming, de-furring of cattle, sheep and goats with kerosene and tyres (and so many others).
How can Nigerians reduce the chances of developing and dying from cancers?
We recommend more vigilant oversight and legislature for stringent punitive measures. Embracement of better health seeking habits, regular medical check ups to screen for Non Communicable Diseases (NCDs), advice on sedentary lifestyle and diet which is essentially skewed to three quarter fruits and vegetables during one quarter shared between the carbohydrates and protein source.
To ingest more wholesome complex and natural carbohydrates rather than the more processed starch products they order to be associated with being enlightened and bourgeoisie.
Promotion of knowing more how the body work, so people can pay close attention to their bodies and alert their healthcare providers as soon as they notice any abnormal changes.
Regular screening: For breast cancer, they should practice regular ‘self-breast examination two to three days after their period. While they can get vaccinated against the HPV which causes cervical cancer, (between ages nine-14, and up to 26), and ensure regular screening with HPV testing or Pap’s Smear, or Visual Inspection Techniques with Colposcopy.
A Pap smear, also called a Pap test, is a procedure to test for cervical cancer in women. In addition, they should practice general preventive measures such as eating healthy and wholesome meals, maintaining a healthy weight, being physically active, avoid smoking, drinking alcoholic drinks or sugary drinks excessively and unnecessary exposure to radiation, exposure to industrial and environmental toxins, such as asbestos fibers, benzene, aromatic amines, and polychlorinated biphenyls (PCBs) should also be avoided.
Furthermore, in terms of surviving cancer, patients can join support groups that comprise of people who also have a similar condition, so they can support themselves and lend their voices as the theme of this year’s World Cancer Day (WCD), recommends: I am and I will! Each voice counts. To sum up, the key to reducing the number of deaths arising from cancers is early detection and improved access to treatment.
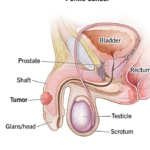
Cancers like prostate, breast and cervical cancers (being acknowledged by the Federal Government to be the three most prevalent cancers in Nigeria), have a better prognosis when they are detected early. And for cervical cancer, with vaccination and vigilant screening, no woman needs to die from cervical cancer. Yet, 26 women still die from cervical cancer!
How about the quagmire of early detection without supporting infrastructure for care and affording management?
Most times, after detection, patients find it difficult to access specialist care because of the limited number of treatment centres within the country and also due to ‘out of pocket payment’ of life threatening crippling medical bills. Little wonders that Nigeria has one of the worst cancer death statistics globally and in Africa. One out of every five persons with cancer die and late detection due to lack of planned and structured screening programmes, no offer to get screened at the point of care, and ‘it is not my portion syndrome’, borne out of fear that cancer is a death sentence, procrastination, and stigmatisation and abandonment by family, especially ‘spousal rejection.’
These issues, inclusive of an available, accessible and affordable health insurance scheme, have to be addressed for a reduction in the number of deaths, ‘survivor population’ or people living with cancer.
What is the impact of air pollution on the burden of cancer in Nigeria?
Air pollution leaves our lungs in a permanent state of inflammation and could possibly increase risk of coming down with serious complications of COVID-19. In a CNN interview, Dr. Maria Neira, WHO Director, Department of Public Health, Environmental and Social Determinants of Health, opined: ‘The contributing factors to pollution are a reliance on using solid fuels for cooking, burning waste and traffic pollution from very old cars.’
At home, due to unreliable electricity supplies, many Nigerians rely on generators, which spew out noxious fumes, often in unventilated areas. On the street, car emissions go unregulated.
There is no serious roadworthiness oversight of vehicles in Nigeria, and the little there is owners bribe their way across regulators.
Neira added: “In Africa, unfortunately, the levels of pollution are increasing because of rapid economic development and industry without the right technology.”
Even those working with paint, etc, with no protection for their workers predispose them to cancers.
So what are you doing to reverse the situation?
Our Non Governmental Organisation (NGO), Breast Without Spot (BWS) focus for 2021 is to contribute to the global call for cervical cancer elimination in Nigeria. We intend to do this by providing online help desk complemented by a ‘BWS NGO’ dedicated App custom built to efficiently navigate women who through our media jingle advocacy, want to respond to the call to: get vaccinated and get screened for early detection of cervical cancer. Planning and implementation are about 65 per cent accomplished, and it had been our target to launch this BWS ‘jingle/help -desk’ cervical cancer elimination programme and roll out on this 2021 World Cancer Day, but alas, our Key Performance Indicators (KPIs), fell short of our expectations, due to some logistics constraints, resulting from the unanticipated second wave of COVID-19! Our new take off, is March/April 2021!
How does BWS help cancer patients to survive?
BWS’ main strong point is leading Go Pink Campaigns, which earned her founder the alias name of Pink Prof. Thus our mass advocacy campaigns such as: the yearly October 5, ‘Nationwide Go Pink Day’ instituted since 2015; and cancer patient treatment fund’ to assist indigent patients pay their bills (since 2018).
There is also the BWS cancer prevention advocacy with NYSC army of advocates that play the role of disseminating cancer control information throughout the 774 Local Government Areas (LGAs) in the country (as our target with an accompanying training manual for the advocates, instituted since 2009.
We also have BWS community screening outreaches. BWS has the structure/infrastructure, to motivate/community mobilise, / screen up to 5,000 to 10,000 women and men and to vaccinate and to treat pre-malignant cervical lesion in any community in Nigeria! Previous clients are State governments, philanthropic organisations, other Civil Society Organisations (CSOs), Federal Ministry of Health (FMOH) and Faith Based Organisations (FBOs). This is one of BWS strongest backbones.
There is also BWS well being and lifestyle consultation and master classes; capacity building screening; skills transfer hands-on workshops; biomedical research and clinical trials; and innovation of the International Cancer Week in Nigeria, by BWS founder, which is currently a Federal Ministry of Health (FMoH) driven annual event in Nigeria.
Are there cures for cancer?
There are so many medications available with different stages of the tumour biology to see if cure can be achieved. Some Nigerian bench scientists have some candidate products that from their studies suggest potential to treat cancers.
Our recommendations are that Nigerian government should henceforth be proactive in providing funds for clinical trials, to take the bench studies through to the bedside and to the market place.