
Malaria has been described as Nigeria’s most enduring public health challenge. Caused by parasites of the genus Plasmodium, the disease remains a leading cause of mortality, with Nigeria bearing the highest malaria burden globally. In fact, Nigeria is responsible for 27% of the world’s malaria cases. Its economic impact is also costly, with the country losing 1.1 billion dollars annually to the disease.
According to the World Health Organization, malaria was the cause of death for 597,000 people in 2023 alone, disproportionately affecting children under the age of five.
One of the growing challenges to the treatment of malaria is the antimicrobial resistance developed by malaria parasites due to mutation – a phenomenon whereby the DNA of an organism goes through a permanent change. Over time, the malaria parasite has developed resistance to previously effective drugs such as chloroquine, sulfadoxine-pyrimethamine, and, more recently, artemisinin-based combination therapies (ACTs), the current standard treatment.
For a country like Nigeria, whose Northern and Northeastern regions experience the highest incidence of malaria, drug resistance is significantly hindering malaria prevention efforts in the country. Addressing this challenge requires innovative scientific solutions, such as the research currently being conducted at the Prof. Neta Regev-Rudzki Malaria Laboratory at the Weizmann Institute of Science, Israel.
The Laboratory is investigating the potential of synthetic Antimicrobial Peptides (AMPs) in combating drug resistance. This research is led by Edo Kiper and Daniel Ben-Hur, PH.D researchers at the Weizmann Institute of Science, Israel. Antimicrobial Peptides (AMPs) are essential players in the innate immune system, acting as the first line of defense against a wide range of pathogens. These peptides come in all shapes and sizes, varying in length, sequence, and structure. Since natural antimicrobial peptides are integral to the immune systems of all biological life forms, scientists at the Neta Regev-Rudzki Malaria Laboratory are exploring how these properties can be replicated synthetically to combat malaria more effectively.
To begin this study, the efficacy of the peptides in eliminating Plasmodium parasites in infected red blood cells was tested. An experiment was set up to precisely assess the anti-Plasmodium falciparum (Pf) activity of various synthetic AMPs. To get the exact peptides with potential anti-Pf activity, a selection of AMPs (at a concentration of 12.5 μM) was incubated with synchronized trophozoite-stage Pf parasites for 24 hours. The growth inhibition was then evaluated using flow cytometry with three independent biological replicates. The results identified five synthetic AMPs—Amp1D, C3, C4, C5, and C6—that significantly reduced Pf growth, resulting in a notable decrease in parasitemia. Importantly, these peptides exhibited minimal hemolytic activity on uninfected Red Blood Cells (RBCs), which is a key factor in ensuring their safety. These synthetic AMPs were also identified as well-performing candidates for future drug development and other applications in biomedical sciences.
 Since natural antimicrobial peptides are integral to the immune systems of all biological life forms, scientists are exploring how these properties can be replicated synthetically.
Since natural antimicrobial peptides are integral to the immune systems of all biological life forms, scientists are exploring how these properties can be replicated synthetically.
These findings open up new possibilities for treating malaria, especially as the disease becomes more resistant to drugs. This research showed that synthetic AMPs, due to their reduced likelihood of resistance development, could offer a groundbreaking approach to anti-malaria treatment. Their low hemolytic activity, excellent safety profile, and resilience against proteolytic degradation suggest they could be safely used in the human body, with a sufficiently long half-life to be effective against pathogens. Plus, their effect on the malaria parasite’s membrane could help slow down resistance, which is a big challenge in the fight against malaria.
This study lays the groundwork for future research on using AMPs as a delivery system for anti-malaria drugs. The selective nature of AMPs, particularly Amp1D, offers the possibility of targeting Pf-infected RBCs while sparing healthy cells. This ability to distinguish between infected and uninfected cells positions AMPs as promising candidates for drug delivery vehicles. Combining Amp1D with anti-malaria drugs could make the drugs more effective and reduce side effects. This discovery brings us closer to developing a new type of malaria treatment that could be a game-changer in fighting the disease.
A key contributor to this groundbreaking research is Kator Igbudu, Coordinator of the Public Health Programme in the School of Allied Medical Sciences at Miva Open University. Mr. Igbudu participated in the Bridges of Science (BoS) programme, a prestigious initiative of the Weizmann Institute and the International Master of Public Health Programme (IMPH) of the Braun School of Public and Community Medicine, Hebrew University of Jerusalem, which offers an exceptional research opportunity to outstanding alumni of the IMPH from Sub-Saharan Africa.
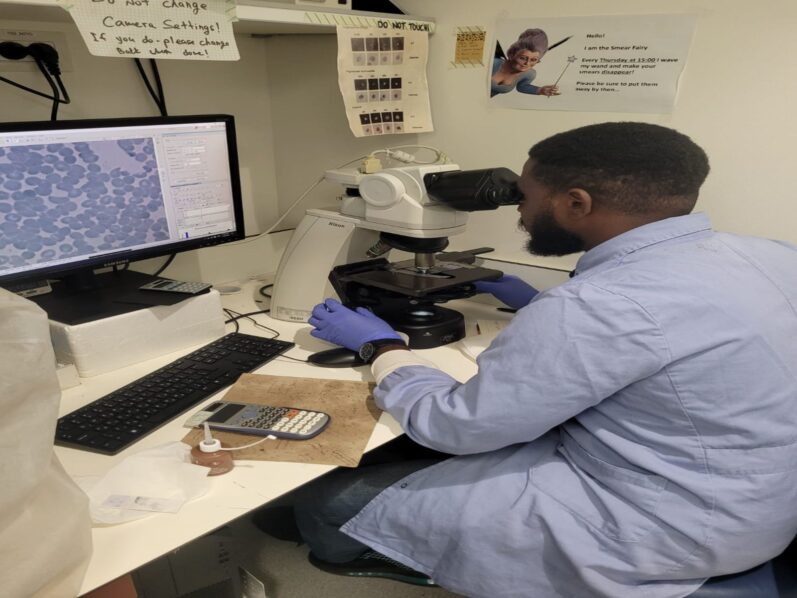
 Kator Igbudu at the Weizmann Institute of Science, Israel
Kator Igbudu at the Weizmann Institute of Science, Israel
Beyond his research contributions, Mr Igbudu has an extensive track record in public health advocacy and intervention. He has a Bachelor of Science in Public Health from the University of Calabar and a Master of Public Health from the Braun School of Public Health and Community Medicine, Hebrew University of Jerusalem. Mr Igbudu has been involved in public health interventions focused on HIV and malaria prevention and treatment, as well as providing first-line support to survivors of gender-based violence—an urgent public health concern among individuals at risk of or living with HIV. His passion for this line of work comes from the huge burden these diseases impose on Nigerians.
With continued scientific advancement and institutional support, innovative solutions like synthetic antimicrobial peptides could offer a new way to fight against malaria. As research progresses and new discoveries emerge, the possibility of more effective treatments becomes increasingly within reach. A future where malaria is no longer a leading cause of death in Nigeria is not just a hope—it is an achievable goal, driven by relentless scientific inquiry and the pursuit of solutions that can transform lives.

![Lab 4[1]](https://guardian.ng/cdn-cgi/image/format=auto,width=600,fit=contain,q=70/https://cdn.guardian.ng/wp-content/uploads/2025/04/Lab-41.jpg)




