The Federal Government has launched new national guidelines for the management of postpartum haemorrhage (PPH) in communities and health facilities, alongside a labour care guide and community-use guidelines for Misoprostol, aimed at reducing preventable maternal deaths.
Under the new framework, the government will implement a Sector-Wide Approach through the Decentralised Facility Financing (DFF) package, targeting at least 7 million pregnant women and 6 million births annually.
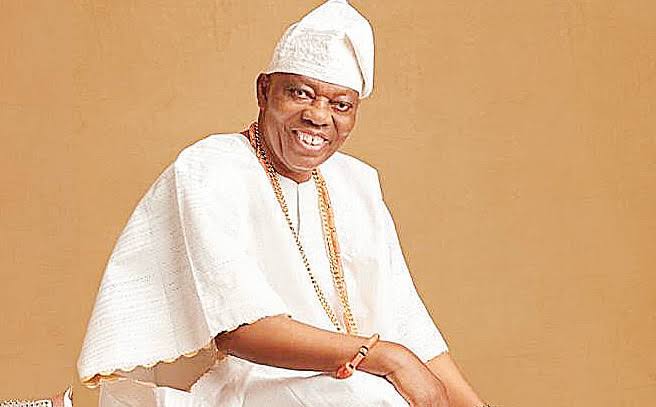
Minister of Health and Social Welfare, Prof. Muhammad Pate, who unveiled the documents in Abuja, decried the persistently high rates of maternal and newborn deaths in the country, noting that most are preventable with timely and quality care.
Pate identified postpartum haemorrhage, excessive bleeding after childbirth, as a leading cause of maternal mortality in Nigeria and globally.
He added that newborn mortality, often due to birth asphyxia and complications of prematurity, also remains a major concern. “Safe motherhood is achieved when every pregnant woman receives all the pillars of care, full antenatal services, skilled and safe facility-based delivery, respectful maternity care, and postnatal care integrated with family planning, especially postpartum and post-abortion services,” Pate said.
The minister also introduced the calibrated drape, a new tool designed to facilitate the early detection of PPH through the accurate measurement of blood loss during delivery.
He described the device as a “simple but effective innovation” that has proven to significantly reduce maternal deaths in settings where it has been adopted.
“By incorporating the calibrated drape into maternal health protocols, we can better monitor and manage haemorrhage, ultimately saving the lives of mothers and their children,” he stated.
Pate added that the ministry has forecasted and quantified essential maternal health commodities, including calibrated drapes, to ensure their inclusion in the Logistics Management Information System (LMIS) for procurement, tracking and accessibility.
MEANWHILE, the World Health Organisation (WHO) and leading global reproductive health agencies have also released new guidelines to end deaths from postpartum haemorrhage.
According to WHO, PPH remains one of the world’s leading causes of maternal mortality, accounting for about 45,000 deaths annually and affecting millions of women each year, mostly in low- and middle-income countries, particularly in sub-Saharan Africa and South Asia.
The updated global recommendations, developed by the WHO, the International Federation of Gynecology and Obstetrics (FIGO), and the International Confederation of Midwives (ICM), introduce new objective diagnostic criteria for detecting postpartum bleeding and call for a major shift in prevention, diagnosis, and treatment.
The guidelines stress the need for better prevention, faster diagnosis, and more effective treatment, while also emphasising the importance of addressing underlying risk factors such as anaemia, which increases the likelihood and severity of PPH.
President of FIGO, Prof. Anne Kihara, said the new approach focuses on readiness, recognition, and response, ensuring that health workers can deliver the right care at the right time across different contexts.
“Women affected by PPH need care that is fast, feasible, and effective, driving progress towards eliminating PPH-related deaths,” she said.
Chief Midwife of ICM, Prof. Jacqueline Dunkley-Bent OBE, urged governments, donors, and partners to adopt the new recommendations and invest in midwives and maternal care systems. “With collective action and investment, postpartum haemorrhage can become a tragedy of the past,” she said.