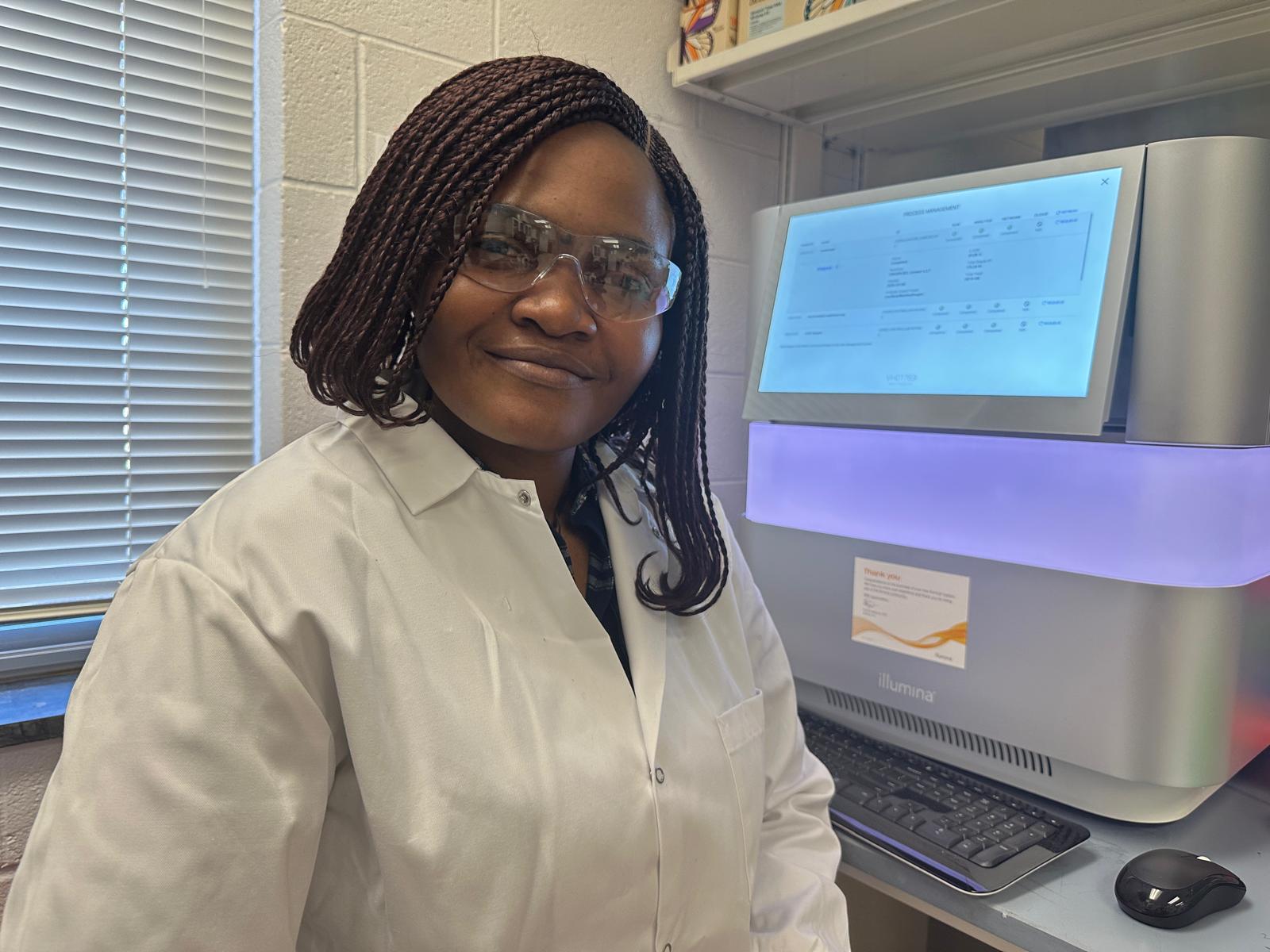
 Public health scientist and Ph.D. researcher, Ugonna Morikwe, is leading the use of artificial intelligence (AI) to track, predict, and combat Antimicrobial Resistance (AMR) in indoor environments and exploring intervention strategies to mitigate their impact on public health. In this interview, Morikwe shares insights into her research on microbial evolution, the challenges and opportunities of bacteriophage therapy, and the urgent need for stronger AMR surveillance in Nigeria. She also shares insights on how interdisciplinary research, spanning infectious diseases, cancer treatment, and natural product therapeutics, can offer holistic solutions to public health challenges.
Public health scientist and Ph.D. researcher, Ugonna Morikwe, is leading the use of artificial intelligence (AI) to track, predict, and combat Antimicrobial Resistance (AMR) in indoor environments and exploring intervention strategies to mitigate their impact on public health. In this interview, Morikwe shares insights into her research on microbial evolution, the challenges and opportunities of bacteriophage therapy, and the urgent need for stronger AMR surveillance in Nigeria. She also shares insights on how interdisciplinary research, spanning infectious diseases, cancer treatment, and natural product therapeutics, can offer holistic solutions to public health challenges.
Can you describe the key findings of your research on microbial evolution and its influence on antimicrobial resistance in built environments?
My research explores how microbial evolution in built environments shapes antimicrobial resistance (AMR) and disease outcomes. Currently, at North Carolina A&T State University in the Jeffers-Francis Laboratory (JF Lab), I focus on profiling microbial communities in indoor environments to understand how antimicrobial exposure and environmental factors drive resistance. The buildings where we live, work, learn, and relax greatly impact our health, well-being, and productivity. Over the years, human activities have increasingly shifted from outdoors to indoors, this shift has not only altered human interactions with the natural world but also reshaped microbial exposures, hence the evolution and variation of microbial communities in indoor spaces.
AMR originating from nosocomial infections is now being detected in non-clinical environments, where resistance is evolving at a rapid pace. In my current study, I focus on profiling microbial communities in homes, to distinguish between pathogenic microbes that cause diseases and beneficial microbes that promote health; by identifying these microbes, we can understand the balance needed for a healthy indoor microbiome. This research reveals how the microbiome’s resilience against pathogens without relying on chemical antimicrobials can play a key role in minimizing antimicrobial resistance.
How do you integrate artificial intelligence into pathogen characterisation, and what are the potential impacts of this approach on public health?
The ongoing arms race between antibiotics and resistant bacteria can be shifted in favour of antibiotics through AI-powered models, I integrate advanced microbiological techniques, traditional methods, molecular approaches, and high-throughput sequencing, to train AI models. I use these models to predict pathogen evolution and AMR trends. These models analyze vast datasets of microbial genomes and environmental factors to identify resistance patterns and help develop targeted interventions.
One major application is in bacteriophage therapy, where machine learning algorithms determine which bacteriophages are most effective against drug-resistant bacterial strains. By leveraging AI, we can improve precision in AMR surveillance, enhance antimicrobial stewardship, and contribute to developing scalable public health strategies.
Your work involves studying bacteriophage therapy. What challenges and opportunities do you see in using bacteriophages to combat antibiotic-resistant infections?
Bacteriophage therapy is a promising alternative to traditional antibiotics, especially against multidrug-resistant bacteria. However, challenges include regulatory hurdles, variability in phage-host interactions, and the need for personalized treatment approaches. The opportunities lie in using AI to optimize phage selection, improving phage-antibiotic synergy, and advancing phage therapy as a viable clinical treatment.
Could you elaborate on the implications of your research on antimicrobial resistance in wastewater and indoor microbiomes for public health policies?
Wastewater serves as a reservoir for resistant genes, reflecting the community’s AMR burden. My research examined the prevalence of AMR genes, virulent factors and pathogenic bacteria in wastewater and indoor microbiomes, providing critical data for public health interventions. Findings from this work can guide policies on antibiotic stewardship, wastewater treatment improvements, and environmental surveillance programs to mitigate AMR risks.
Your master’s work on Plasmodium species highlighted mechanisms of drug resistance in malaria. How do you think lessons from combating malaria can be applied to tackling resistance to other diseases?
In my master’s research under Prof. C.O Esimone, I assessed the prevalence of Plasmodium falciparum infections, evaluated knowledge, attitude, and practices (KAP) related to malaria prevention and treatment, and analyzed molecular markers associated with malarial drug resistance. The study revealed a high prevalence of malaria, poor health-seeking behaviors, and sustained drug pressure from quinoline-based treatments despite the ban on chloroquine, alongside emerging threats to artemisinin-based combination therapies (ACTs).
These findings highlight the need for continuous surveillance, stricter drug regulations, and better public health education to prevent resistance. The importance of enforcing drug bans and promoting combination therapies extends beyond malaria and can inform antimicrobial resistance strategies for other infectious diseases.
Considering the current state of antimicrobial resistance and public health challenges in Nigeria, what do you believe are the most urgent steps needed to strengthen research infrastructure and surveillance systems in the country?
In October 2024, the Federal Government of Nigeria launched the Second National Action Plan on Antimicrobial Resistance, a step in the right direction. However, urgent actions are still needed such as establishing a national, coordinated AMR surveillance system that integrates data from human, animal, and environmental health sectors is essential, especially given the weak regulations, chaotic distribution, and unrestricted access to antibiotics that drive resistance. Strengthening laboratory capacity with modern diagnostic tools and well-trained personnel is critical to generate reliable data for informed decision-making. Increased investment in AMR research, along with a centralized data repository, will support consistent monitoring of resistance trends.
Strict enforcement of antibiotic regulations, the creation of antimicrobial stewardship (AMS) teams in hospitals, and administrative support for AMS programs are necessary to improve antibiotic use. Public education on responsible antibiotic use is also key to reducing misuse. Additionally, fostering collaborations among universities, biotech companies, public health agencies, and international organizations will drive innovation and technology transfer. Building a skilled workforce by training epidemiologists, microbiologists, bioinformaticians, and public health professionals specializing in AMR surveillance and outbreak response is vital to strengthening Nigeria’s capacity to manage AMR and protect public health.
As someone deeply involved in organising scientific events like the 2024 Antimicrobial Resistance Conference, how do you plan to use these platforms to foster collaboration and drive actionable solutions for Nigeria’s public health issues?
Through conferences and workshops, I aim to create spaces for cross-sector collaboration, bringing together academic researchers, public health officials, and industry leaders. These events facilitate knowledge exchange, data sharing, and capacity building, particularly for early-career scientists in AMR research and surveillance. They also serve as incubators for policy recommendations and innovative solutions tailored to Nigeria’s public health needs.
Beyond my research, I am a strong advocate for scientific collaboration and graduate student engagement. With over 10 years of mentoring experience, I actively train undergraduate students in microbiological techniques and data analysis to help shape the next generation of scientists tackling emerging microbial threats. Prior to my Ph.D., I served as a Lecturer at Nnamdi Azikiwe University in the Department of Pharmaceutical Microbiology and Biotechnology, where I mentored students in microbiology and AMR solutions.
By leveraging platforms like the 2024 AMR Conference held at the Faculty of Pharmaceutical Sciences, Nnamdi Azikiwe University, I seek to promote interdisciplinary partnerships, strengthen local scientific expertise, and advocate for policy-driven research that directly addresses Nigeria’s AMR challenges and public health priorities.
Your research spans diverse areas, including natural product therapeutics and triple-negative breast cancer (TNBC). How do you balance these interdisciplinary interests, and what connections have you found between them?
Balancing my interdisciplinary interests has been both strategic and organic. These fields intersect through the impact of microbial dynamics on health outcomes, particularly in how antimicrobial exposure influences both infectious disease progression and cancer treatment responses.
In TNBC, patients often undergo antimicrobial treatments that can disrupt the microbiome, fostering the emergence of multidrug-resistant organisms and potentially weakening immune responses critical for cancer control. This highlights a direct connection between AMR and oncology, where microbial imbalances affect both infection susceptibility and treatment efficacy.
My research in natural product therapeutics offers a potential solution by exploring plant-derived bioactive compounds with antimicrobial and immune-modulating properties. These natural products not only serve as alternatives to conventional antibiotics, reducing selective pressure that drives AMR, but also hold promise in combination with bacteriophage therapy to target drug-resistant bacteria more effectively. Given that phages and certain natural compounds can work synergistically to disrupt bacterial biofilms and enhance bacterial clearance, this approach may improve infection management in TNBC patients while minimizing microbiome disruption.
By integrating these fields, I design research that addresses real-world challenges, such as identifying resistance patterns in TNBC patient microbiomes and evaluating alternative therapeutics to combat infections without exacerbating AMR. This interdisciplinary approach enhances my ability to contribute to both infectious disease management and improved cancer treatment outcomes.
What strategies do you believe are most effective for fostering collaboration among researchers to address antimicrobial resistance at the intersection of healthcare and environmental settings?
Fostering meaningful collaboration requires creating platforms that encourage interdisciplinary dialogue and shared problem-solving. One key strategy I employ is organising workshops, symposia, and training sessions that bring together researchers from diverse fields such as microbiology, public health, environmental science, and clinical practice.
In my leadership role as Vice President and Chair of Academic Affairs for the Graduate Student Association at North Carolina A&T State University, I work to expand research opportunities for graduate students and facilitate professional development through events like the Annual Graduate Research Symposium. These initiatives create opportunities for early-career scientists to engage in interdisciplinary conversations around global scientific challenges, including antimicrobial resistance.
By building these collaborative spaces, we can strengthen research networks that integrate healthcare and environmental perspectives, promote knowledge exchange, and drive innovative solutions to address AMR on multiple fronts.
What specific steps do you hope to take in the next five years to bridge the gap between your scientific research and effective policy implementation, both locally and globally, to improve public health outcomes?
In the next five years, I plan to expand my research on antimicrobial resistance (AMR) surveillance and microbiome health into policy-driven frameworks, both locally and globally. By collaborating with public health agencies, contributing to evidence-based guidelines, and promoting microbiome-sparing antimicrobial strategies, I aim to translate scientific insights into practical solutions.
Presenting my work at international conferences and being invited for talks has allowed me to engage with global experts, policymakers, and researchers, creating opportunities to share findings, influence discussions on AMR management, and build collaborative networks that support policy implementation. These platforms are essential for scaling up interventions and ensuring that research informs real-world practices, particularly in resource-limited settings.
Beyond academia, my work has significant implications for global health. By contributing to scalable intervention strategies, such as probiotic-based environmental modifications, my research is paving the way for sustainable approaches to reducing AMR in low-resource settings. These findings are expected to inform both policy and practice, playing a critical role in curbing the rise of antibiotic-resistant infections and protecting vulnerable populations. With a strong foundation in microbiology, bioinformatics, and public health, I strive to apply scientific inquiry to real-world challenges, ensuring that my research, advocacy, and mentorship collectively shape the future of AMR mitigation and global health equity.
Ultimately, my motivation comes from a deep desire to apply science to real-world problems, mentor the next generation of researchers, and contribute to sustainable public health solutions globally.






