• Workplaces, Public Facilities Should Provide Safe Spaces, Says Health Minister
• Researchers Highlight Benefits, Task Govt On Favourable Policies
August 1-7 is World Breastfeeding Week (WBW). The World Health Organisation (WHO) and United Nations Children’s Fund (UNICEF) promote exclusive breastfeeding for the first six months of a child’s life to reduce the risk of infant mortality from common childhood illnesses such as diarrhoea or pneumonia as well as help babies recover more quickly from illnesses. It also has economic and many health benefits, including reducing adult obesity and non-communicable diseases such as diabetes and hypertension. Despite these benefits, most Nigerian nursing mothers do not practice exclusive breastfeeding due to several challenges. In this report, CHUKWUMA MUANYA and NKECHI ONYEDIKA analyse these obstacles and proffer how to achieve 65 per cent exclusive breastfeeding in Nigeria by 2025.
Investigations have revealed that there are many issues that may arise when a baby is born that could make exclusive breastfeeding challenging for the mother. These include beliefs and practices associated with breastfeeding or if the baby is born sick and has to spend time in an incubator. It is also the case when a woman delivers her baby through Caesarean Section (CS) and if the mother is living with Human Immuno-deficiency Virus (HIV) that causes Acquired Immune Deficiency Syndrome (AIDS).
Diamond Okeke, a Human Resource Manager in a pharmaceutical company in Lagos, shared her personal experience after having her first born and the challenges she faced while breastfeeding.
Her words: “My husband and I planned to exclusively breastfeed our baby. After birth, the nurses helped me to initiate breastfeeding. By the second day it was apparent that the breast milk was not flowing freely and my baby was never satisfied. She was always crying for more, which she was not getting. When my mother came, she ignored the advice of the nurses and introduced water, saying that the baby was not getting enough. By the third day, my mother also introduced infant formula, saying that my breast was not producing enough milk. That was how my plans to exclusively breastfeed my baby failed.”
Indeed, the accounts of breastfeeding experience by women sampled by The Guardian Weekend were characterised by difficulties ranging from physical discomfort to pain and engorgement, as well as emotional distress, body image concerns and loss of independence.
“The pain and the pain of the incision (from Caesarean section) were just the things that made me emotional. But the fact is that I really wanted to breastfeed my baby and I did not want to use the pains as an excuse not to breastfeed my baby. So, I was still breastfeeding even in the pains; you just find yourself crying sometimes, you just cry…,” Mrs. Favour Adepoju said.
Similarly, most of the women felt tied down by breastfeeding with loss of freedom to move around, restrictions to activities, restrictions to fashion/style; expressing concerns over not dressing appropriately in order to breastfeed, particularly in public. For some women, there were anxieties about how breastfeeding would affect the shape of their breasts leading to concerns about remaining sexually attractive to their husbands.
However, while some acknowledged these difficulties, they still prioritised breastfeeding. “I had concerns but I felt breastfeeding is more important than me losing the shape of my breasts,” Mrs. Aisha Abubakar said.
Thus, these difficulties generally did not deter the women from breastfeeding, given their quest to meet social and cultural expectations and to prove themselves as good mothers especially with a prized first infant. Suckling was reinforced by their families and local communities who provided approval and practical support.
However, while most women sampled ahead of the World Breastfeeding Week (WBW) were able to breastfeed their babies despite the challenges they faced, only few were able to practice exclusive breastfeeding (EBF) – putting the baby only on breast milk for the first six months of life.
Exclusive breastfeeding, therefore, means that the infant receives only breast milk – directly from the breast or expressed – without the addition of other liquids or solids, not even water, except oral rehydration solutions, medicines, vitamins or minerals. According to the latest figures from UNICEF, 90 per cent of mothers in Nigeria breastfeed their children but of this number, only 34 per cent exclusively breastfeed their babies within the first six months of their birth as at 2022. This represents an improvement when compared to 19 per cent and 29 per cent recorded in 2020 and 2021 respectively.
The National Policy on Food and Nutrition (NPFN) in line with the World Health Assembly (WHA) targets to increase exclusive breastfeeding rate from 17 per cent in 2013 to 65 per cent by 2025.
Supported by the WHO, UNICEF and many Ministries of Health and civil society partners, WßBW is held in the first week of August every year. In 2018, a World Health Assembly resolution endorsed WBW as an important health promotion strategy. With a different theme each year, it seeks to promote the enabling environment that help women to breastfeed – including support in the community and the workplace, with adequate protections in government policies and laws as well as sharing information on breastfeeding benefits and strategies.
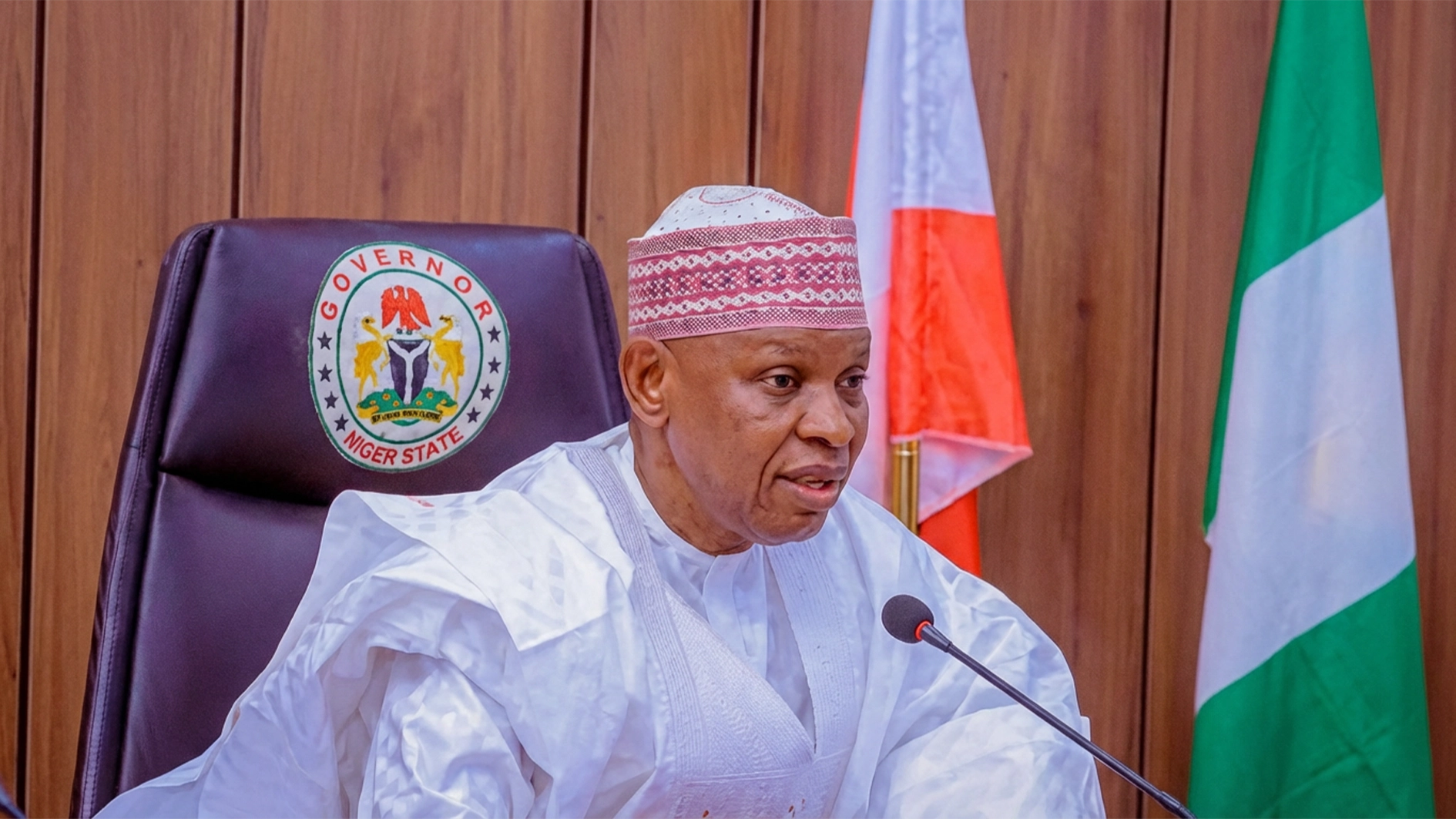
The theme for this year’s WBW is ‘Closing the Gap: Breastfeeding Support for All’. Coordinating Minister of Health and Social Welfare, Prof. Muhammad Ali Pate, in an exclusive interview with The Guardian Weekend, said breastfeeding has multiple benefits, including fostering early mother-child bonding, nourishment of the newborn by colostrum, protection of the child by antibodies in the mother’s milk and diverse nutrients.
“It is crucial for children’s nutrition in the first six months when it should be exclusive,” Pate said. He said the Federal Ministry of Health and Social Welfare has been promoting the practice of breastfeeding as crucial for children’s health and wellbeing.
“We are advocating that every workplace should make provision of safe spaces for breastfeeding mothers as well as in public facilities. This will encourage mothers to practice it and help us build a generation of healthy, well nourished children,” Pate said.
The minister said the Federal Government has lined up a series of activities to mark this year’s WBW, which is aimed at promoting awareness and public support for breastfeeding.
In a statement issued last Monday by the Ministry of Health and Social Welfare, the spokesperson, Patricia Deworitshe, said the country acknowledges the importance of protecting the interest of vulnerable mothers in need of assistance with breastfeeding their offspring.
Deworitshe said the ministry, in collaboration with some of its concerned parties in the sector, would participate in the global campaign from August 1 to 7.
She said: “The week will be flagged off on August 1 with a record-breaking event for most lactating women breastfeeding simultaneously. During the week, the ministry also intends to carry out community outreach across the country, training for health workers and media campaigns.”
She said the global theme for the campaign emphasises the collective responsibility to ensure that every mother receives the support she needs to make breastfeeding a successful and fulfilling experience.
Also, as part of efforts to initiate and sustain exclusive breastfeeding worldwide, UNICEF and Global Breastfeeding Collective will, on August 6, host a virtual meeting on ‘Strength in Numbers – How Monitoring Breastfeeding Policies and Programmes Creates Accountability and Empowers Change’. The Global Breastfeeding Collective is a partnership of more than 20 prominent international agencies, including the WHO and UNICEF, which calls on donors, policymakers, philanthropists and civil society to increase investment in breastfeeding worldwide.
UNICEF and WHO recommend that breastfeeding be initiated within the first hour of life and that EBF should be continued for the first six months of life. The midwives in health facilities give this social behaviour change and communication message to first-time mothers during antenatal clinic attendance. Mothers are also advised that after the first six months, infants are expected to receive safe and nutritionally adequate complementary feeds while continuing to breastfeed up to two years or beyond in order to meet their growing nutritional needs.
According to a new study published in May this year in the open-access journal PLOS ONE by Tomi Ajetunmobi of the Glasgow Centre for Population Health, Scotland, and colleagues, breast milk can promote equitable child health and save healthcare costs by reducing childhood illnesses and healthcare utilisation in the early years.
In the new study, researchers used administrative datasets on 502,948 babies born in Scotland between 1997 and 2009. Data were available on whether or not infants were breastfed during the first six to eight weeks, the occurrence of 10 common childhood conditions from birth to 27 months, and the details of hospital admissions, primary care consultations and prescriptions.
Among all infants included in the study, 27 per cent were exclusively breastfed, nine per cent mixed fed and 64 per cent formula fed during the first six to eight weeks of life. The rates of exclusively breastfed infants ranged from 45 per cent in the least deprived areas to 13 per cent in the most deprived areas.
The researchers found that within each quintile of deprivation, exclusively breastfed infants used fewer healthcare services and incurred lower costs compared to infants fed with any formula milk. On the average, breastfed infants had lower average costs of hospital care per admission (£42) compared to formula-fed infants (£79) in the first six months of life and fewer General Practitioner (GP) consultations than formula-fed infants. At least £10 million of healthcare costs could have been avoided if all formula-fed infants had instead been exclusively breastfed for the first six to eight weeks of life, the researchers calculated.
The authors concluded that breastfeeding has a significant health and economic benefit and that increasing breastfeeding rates in the most deprived areas could contribute to the narrowing of inequalities in the early years.
Also, immediate Kangaroo Mother Care (KMC) reduces the risk of sepsis among small and preterm babies, according to a new analysis published in the medical journal, eClinicalMedicine. Among these vulnerable newborns, immediate KMC – which combines skin-to-skin contact with exclusive breastfeeding or provision of breast milk – reduced suspected sepsis by 18 per cent, sepsis-related deaths by 36 per cent, and overall deaths by 25 per cent.
Conducted by WHO and several external investigators, the secondary analysis assessed data from the immediate KMC study that took place between 2017 and 2020. This study was conducted in five Newborn Intensive Care Units (NICUs) in Ghana, India, Malawi, Nigeria and Tanzania in newborns with birth weight ranging from one to 1.8 kilogramme. The study compared outcomes for babies where KMC was initiated immediately after birth, compared to babies who received conventional care in a warmer or incubator followed by KMC only, once clinical stabilisation was achieved.
The analysis adds to evidence showing the incredible benefits of immediate KMC for small and preterm babies, including improved survival, lower infection rates, reduced hypothermia and better feeding.
For all preterm or low birth weight babies – including babies that are very small or sick – the WHO recommends starting KMC as soon as possible after birth. For many health facilities, this will require a fundamental change in the way neonatal care is provided to ensure families and small babies can stay together, without any period of separation.
Meanwhile, results of a comparative study of exclusive breastfeeding between mothers of formal and informal sector workers in Ede North Local Council of Osun State showed significant difference in knowledge and practice of exclusive breastfeeding between formal and informal sector workers.
According to the study published recently in the International Journal of Community Medicine and Public Health, factors affecting exclusive breastfeeding include lactation, job hindrances and crèche availability. The practice of exclusive breastfeeding was low among mothers in the formal sector, and the factors impacting its practice reported in this study may have substantial implications for breastfeeding intervention programmes.
The researchers from the Departments of Public Health and Physiology, Adeleke University, Ede, Osun State, and California Department of Corrections and Rehabilitations, San Diego, United States, concluded: “As a result, attempts to promote EBF should target specific populations of informal sector women and areas where it is underutilised. Moreover, mothers must be supported. Furthermore, mothers should be encouraged to attend antenatal care where they will learn about the benefits of exclusive nursing to children under the age of six months, allowing them to make informed decisions on exclusive breastfeeding.
“The Nigerian government should ensure that the Employment Act’s maternity leave benefits are implemented in the informal sector, allowing women to practice EBF.”
In a study on lived experiences of first-time mothers with exclusive breastfeeding in Kafue, Zambia, published in Nurse Care Open Access Journal, three major themes emerged: Challenges Initiating and Continuing Breastfeeding; Psychological Aspects of EBF Practice in Relation to Coping and Inadequate Support Networks/Mechanisms.
The study found that first-time mothers experienced diverse challenges with EBF and information received from healthcare providers did not prepare or help them adequately. Practical support was received from nurses and midwives, however only in the first six weeks postpartum. In some instances, support was either not given or it was not supportive of EBF.
“Given their inexperience, first-time mothers experience EBF challenges that are difficult to deal with leading to very negative effects on their perceptions of EBF thus negatively affecting EBF practices. Without adequate and appropriate practical support in the perinatal period, they are most likely not to EBF successfully. Teaching on danger signs of breastfeeding complications and incorporating breastfeeding clinics in the Maternal and Child Health Departments could be utilised as strategies to help them sustain successful EBF practices,” the researchers concluded.
Indeed, initiation of breastfeeding within an hour after delivery has been shown to increase the chances of breastfeeding and extending the length of breastfeeding; consequently improving the rates of EBF even for first-time mothers. Furthermore, continuing to EBF without giving any other food is said to promote sensory and cognitive development, as well as protecting infants against infectious and chronic diseases. Early initiation of breastfeeding immediately after birth promotes bonding between a mother and her baby thereby enhancing the success of breastfeeding, providing warmth and security for the new-born baby.
Globally, studies on the cognitive, psychological, physiological, social development and economic benefits of breastfeeding show that breastfeeding is superior to any other method of infant feeding and provides benefits to babies, mothers, their families, communities and nations in each of the areas studied. Breastfeeding offers long and short-term benefits for the mother and the baby. Breast milk has all the nutrients required by the baby in the right proportions and changes according to the baby’s changing nutritional needs especially in the first month of life. Over 200 different nutritional components are contained in the human breast milk, which makes breast milk the perfect sustenance for infants. It is estimated that along with economic savings of US$300 billion, deaths of approximately 823,000 children and 20,000 mothers (due to breast cancer) worldwide could be avoided through optimal breastfeeding practices each year.
EBF is the most cost effective intervention to reduce infant mortality. This is because it has shown a reduction in childhood illnesses such as diarrhoea and pneumonia (the two primary causes of child mortality worldwide), middle ear infections (by 50 per cent), respiratory infections (72 per cent) and intestinal tissue damage (60 per cent). It also protects infants from sudden infant death syndrome by 50 per cent in the first month and 36 per cent in the first year, allergic diseases (27-42 per cent), celiac diseases (52 per cent), inflammatory bowel disease (30 per cent) and childhood leukaemia (by 15-20 per cent). Breastfed premature and low birth weight infants are equally protected from necrotising entero-colitis.
In addition to reducing the risk of infections, breastfeeding has been shown to reduce their severity and duration; saving approximately 1.5 million infants worldwide yearly. This is because breast milk, particularly colostrum, has antibodies and proteins which provide initial immunisation making it less likely for infants to develop allergies and other conditions (example, eczema, asthma). Colonisation of the gut by a variety of microbiota protects breastfed infants from infections such as Salmonella, Listeria and Campylobacter. In 2014, UNICEF also established that breastfed babies in developing countries were at least six times more likely to survive in the first month of life than non-breastfed babies.
Extensive evidence has further shown that breast milk has a role to play in brain development. EBF is linked to better performance and higher Intelligence Quotients (IQs) in breastfed than non-breastfed children. The difference could be linked to the physical intimacy, touch and eye contact associated with breastfeeding. This is even more significant in preterm babies who have a higher risk for developmental issues. EBF is further associated with better growth and development of infants thereby contributing towards a reduction in stunting.
Evidence further shows that breastfeeding is not only beneficial to infants, but also their mothers. A critical review of epidemiological studies demonstrates the short and long-term effects of breastfeeding to the mother, which include early return of the uterus to its pre-gravid state through oxytocin release in the postpartum period. Early initiation of breastfeeding soon after the baby is born is also associated with decreased risk of postpartum haemorrhage. It enhances the release of oxytocin, promoting relaxation and reducing psychological as well as emotional stress and postpartum depression. Frequent infant suckling also stimulates the release of prolactin, which in turn stimulates milk production and secretion. EBF is also associated with reduced risk of breast, ovarian and endometrial cancer during the premenopausal period. Furthermore, longer duration of breastfeeding shows reduced risk of type-2-diabetes; high blood pressure, increased cholesterol level, breast cancer, uterine and ovarian cancer.
Additionally, research studies have reported frequent night time breastfeeding as an effective natural contraceptive because it has the tendency of delayed menstruation (Lactation Amenorrhea Method) and consequently a well-planned family.
Can mothers living with HIV breastfeed? “If you are a woman living with HIV in an area of the world where access to resources such as clean water, refrigeration and medical care is limited, the WHO recommends that you breastfeed if you are taking HIV drugs. A course of HIV drugs may also be recommended for the baby during breastfeeding. One reason for this recommendation is that in such settings (for instance, many areas of Africa or India), infants are more likely to develop diarrhoea and other illnesses, and may die from these,” said Dr. Murphy Akpu of Joint United Nations Programme on HIV/AIDS (UNAIDS).
According to Akpu, breast milk contains substances that protect and strengthen a child’s immune system, even after they stop breastfeeding.
“Because of this, breast milk may help children to survive these health conditions. Furthermore, formula feeding may not be an option in these areas because of lack of money to buy it, clean water to mix it with (if the formula is powdered) or refrigeration to keep it fresh. Health authorities have determined that the benefits of breastfeeding outweigh the risk of HIV transmission in areas where resources are limited,” he said.