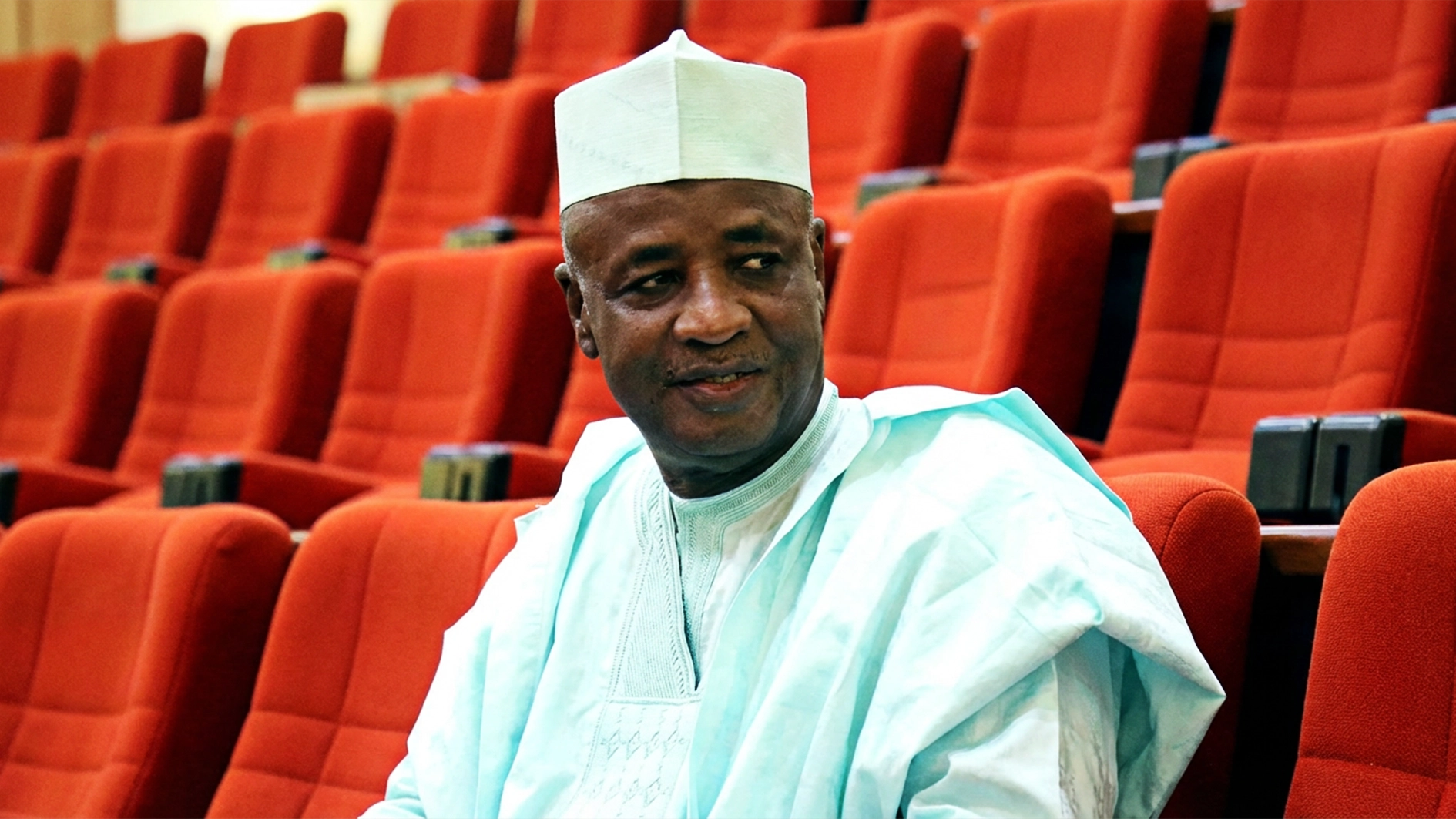
Amid the growing concerns surrounding chronic kidney disease (CKD) and its connection to cardiovascular health, a leading expert in the field, Dr. Emeka Obi, has hinted at breakthrough findings that could redefine patient care in both disciplines. Dr. Obi, a pioneering researcher, has made significant strides in understanding the complex relationship between CKD and cardiovascular events, revealing insights that could transform clinical approaches.
Amid the growing concerns surrounding chronic kidney disease (CKD) and its connection to cardiovascular health, a leading expert in the field, Dr. Emeka Obi, has hinted at breakthrough findings that could redefine patient care in both disciplines. Dr. Obi, a pioneering researcher, has made significant strides in understanding the complex relationship between CKD and cardiovascular events, revealing insights that could transform clinical approaches.
Speaking with newsmen at the Nigerian Medical Association 63rd annual general meeting, Dr. Obi highlighted the importance of his team’s findings.
He noted that, “Our groundbreaking study has uncovered key predictors of cardiovascular events among CKD patients, such as malnutrition, post-dialytic hypotension, thrombophilia, and post-transplant immunosuppressive therapy. These findings are crucial in helping physicians tailor treatment strategies and prioritize interventions for improved outcomes.”
According to him, CKD continues to affect millions of people worldwide, significantly increasing the risk of cardiovascular complications such as heart failure, sudden cardiac death, and acute coronary syndromes. “The staggering incidence of adverse cardiovascular events, estimated at 158 per 1000 CKD-related hospital admissions, highlights the urgent need for more refined management strategies,” Dr. Obi explained.
Dr. Obi’s research is particularly notable for its comprehensive analysis of over 690,000 hospitalizations. This massive dataset allowed his team to pinpoint CKD-specific risk factors that had previously been overlooked or underemphasized in clinical settings. Malnutrition, for instance, emerged as a critical predictor of poor cardiovascular outcomes, shedding light on the importance of nutritional status in CKD management.
Another crucial factor identified was post-dialytic hypotension, which, according to Dr. Obi, exacerbates the risk of cardiovascular events in CKD patients. “Understanding how these risk factors interplay allows for more effective prevention and treatment of cardiovascular events in this vulnerable population,” he added. Thrombophilia and sleep disorders also surfaced as significant contributors, further complicating the risk profile for CKD patients.
One of the most impactful aspects of this study is its potential to revolutionize clinical decision-making. Dr. Obi emphasized that the findings would enable physicians to prioritize interventions that target these CKD-specific risk factors, shifting the focus from traditional cardiovascular treatments to a more personalized approach. This could dramatically enhance patient care and improve outcomes in the long run.
The implications of Dr. Obi’s research extend far beyond the clinical setting. He believes that the study serves as a model for interdisciplinary collaboration and rigorous investigation in both cardiovascular and renal medicine. “This study is not just about identifying risk factors; it’s about changing the way we approach treatment, creating opportunities for better integration between specialties,” Dr. Obi remarked.
The study’s findings are also expected to influence healthcare policy, particularly in regions like Sub-Saharan Africa and Nigeria, where the burden of CKD and cardiovascular disease is disproportionately high. Dr. Obi stressed that the research has profound implications for healthcare systems in these regions, where early intervention and tailored treatment strategies could save countless lives.
Dr. Obi’s work inspires a new generation of researchers and clinicians, highlighting the critical need for continued innovation in medical research. By paving the way for further studies, he hopes to see even more groundbreaking discoveries that will continue to reshape CKD management and cardiovascular care.
Perhaps most importantly, this research offers hope to patients and their caregivers. Empowered by the knowledge gained from Dr. Obi’s work, patients can now navigate CKD management with renewed optimism, armed with the tools and strategies needed to reduce cardiovascular risks. “Patients no longer have to face this battle blindfolded; we’re giving them the information they need to make informed decisions,” Dr. Obi stated.
The potential for improved patient outcomes is enormous. With personalized medicine approaches becoming more mainstream, CKD patients at high risk of cardiovascular events could see enhanced quality of life and reduced mortality. “We are entering a new era of personalized cardiovascular care, where each patient’s unique risk profile will guide their treatment,” Dr. Obi noted.
Dr. Obi’s landmark study also underscores the need for enhanced patient-physician communication. He believes that clearer, more open discussions between doctors and patients will be vital to the success of these new treatment approaches. “Good communication is key to ensuring patients understand their risks and treatment options,” he said.
As we embark on this transformative journey, Dr. Obi’s visionary research illuminates the path forward. His findings not only redefine the boundaries of cardiovascular and renal medicine but also inspire a brighter future for CKD patients worldwide. The combination of scientific discovery and practical application makes this research a cornerstone for future innovations.
He noted that the groundbreaking work will reshape the landscape of CKD and cardiovascular medicine by illuminating CKD-specific risk factors and offering new insights into their management.
The implications are particularly profound for regions like Sub-Saharan Africa and Nigeria, where the need for such advances is critical.