A lot of progress has been made by Doctors in the field of infectious diseases. We can bring to remembrance the discovery of anthrax, Tuberculosis, cholera as you remember Robert Koch. The algorithm for the definition of infectious agent of a disease popularly known as Koch’s postulate was developed by Robert Koch(1843-1910). The German doctor also made significant contributions to the development of the first ‘magic bullets’ (antimicrobials i.e chemicals developed to attack specific microorganisms). RobertKoch was awarded a Nobel Prize in 1905 (Lakhtakia 2014). It is heart-warming to remember Gerhard H. A. Hansen. The doctor from Norway who identified the germ that is responsible for leprosy. Under a microscope in 1873, Hansen’s discovery of Mycobacterium leprae proved that leprosy is caused by a germ, and thus not heredity, nor from a curse, nor from a sin.
Initial use of sulfone therapy by Dr. Guy Faget of Carville in1941, the discovery that the footpad of mouse supported the multiplication of M. Leprae was by Dr. Charles shepard of the center for Disease control in 1959 and the demonstration that the nine-banded armadillo is highly susceptible to developing disseminated Hansen’s disease after inoculation with the M. leprae was made by Dr. Waldemar Kirchheimer of Carville and Dr. Eleanor Storrs of the Gulf South Research Institue in 1963. (Leprosy/references2005; Trautman J. R. 1984) In the 18th century in Europe, 400,000 people died annually from smallpox, and one third of the survivors went blind. Jenner’s work represented the first scientific attempt to control an infectious disease by the deliberate use of cowpox to protect people against smallpox. His discovery later led to the eradication of small pox in 1977. (Riedel 2005) The erroneous Aristotelian concept of spontaneous generation (abiogenesis) was prevalent before late 1800. Pasteur (1822-1895) and John Tyndall a Scotland physician (1820-1893) performed experiments that finally silenced the concept of abiogenesis. (Tyndall 1966).
In the words of John Bankston, ‘At a time when surgery couldn’t have been more hazardous, an unlikely figure stepped forward: a young, melancholy Quaker surgeon named Joseph Lister, who would solve the deadly riddle and change the course of history. Lister’s discoveries culminated in his audacious claim that germs were the source of all infection—and could be countered by antiseptics.’ In addition, pure cultures were first obtained by Joseph Lister in 1878 using serial dilutions in liquid media, providing a great boost in infectious diseases’ discovery (Bankston 2004, Stefan 2005) Born of a teacher in Lagow, Germany, Gerhard Domagk completed his medical degree in 1921 and then began an academic career, pursuing research in pathology.
Sulfa drugs, was introduced in 1935 by Gerhard Domagk (1895–1964), to treat bacterial infections. This achievement earned Gerhard Domagk a Nobel Prize (Science History Institute, 2017). By the grace of God, at another time, I will discuss the great work of our living and late Nigerian Microbial Pathology legends in the likes of Professor Adegboro Boaz, Professor Odugbemi, Professor Cooker, Professor Brawart, Professor Bakare and a host of others. I hope to put on record, the achievement of other Professors of Pathology in Microbial specialty including Folashade Ogunsola, Onipede, Chris Nwabuisi, Akanbi II AA, Taiwo SS, EOP Nwokedi, just to mention a few. Erudite scholars and Professors such as Edugbola, LD, Olaleye, Adu, Omilabu AS, Fagbami AH, will never be left out. They have made their marks.
Getting started The Vice Chancellor Sir, for me, efforts at understanding the basis of human diseases and its solutions (Pathology)as it relates to infectious diseases is a call to service. Early shot at infectious diseases researches started from an initial work with Dr Wahab I. Olanrewaju and Prof. WBR Johnson when we looked at why we were having treatment failures with the use of chloroquine as the drug of choice in malaria treatment. From that study, it was uncovered that inappropriate or inadequate dosing and poor compliance constituted a threat to continued clinical effectiveness of chloroquine as injectable chloroquine is not supposed to be the rule in outpatient management of acute uncomplicated malaria.
Treatment failures and of course resistance was due to under-dosing as a result of using 200mg 12hourly for three doses instead of800mg daily for days 1 &2and 400mg on day 3 (expressed as 4-4-2). The problems resulted from over-indulgence in injectable chloroquine. We yielded to societal pressure of preference and confidence in injectable rather than oral medications. The resistance that necessitated the change to Artemisin-based Combination Therapy (ACT) would not have been needed that soon and the cost of managing malaria would not have been as high as it is today (Olanrewaju et al 2002).
In view of the emerging consequences and in line with the World Health Organization (WHO) recommendation, The Federal Ministry of Health in 2005 had to officially adopt ACT as the first line treatment for acute uncomplicated malaria. Following wide incorporation of the change of malarial standard treatment from chloroquine to ACT, our team in malaria research centre, Olanrewaju Hospital, Ilorin evaluated 3 major artemisin-based combinations available in Nigerian market to determine their efficacy and tolerability. We found adequate clinical and parasitological response comparative between artemeter-lumefantrine and atesunate-amodiaquine groups, both combinations being significantly more efficacious than artesunate-sulphadoxine-pyrimenthamine group.
However, drug related adverse effects were significantly higher among atesunate-amodiaquine group compared to other treatment combinations. This provided important guide in management of malaria using ACTs especially among adults. Many years down the line in antimalarial prescription, this finding is still quite relevant in prescription pattern(Olanrewaju, et al 2010). The gold standard for malaria diagnosis is microscopic examination of Giemsa stained thick and thin blood film. The causative agent of malaria are species of plasmodium which include Plasmodium falciparum, P. malariae, P ovale, P vivax. Early In the millennium, rapid diagnostic tools (RDTs) for malaria diagnosis began to penetrate Nigerian market. This was based on the discovery of certain proteins which are specific to plasmodium.
These proteins are his tidine rich protein-2 (hrp-2), aldolase, and plasmodium falciparum specific Lactate dehydrogenase (PFLD). Nigerian market was one of the targets for the new product. It was a welcomed development because as at that time, crisis was brewing in the health sector especially related to personnel in Laboratory Medicine departments. Our people were no longer interested in laboratory bench work as the politics of laboratory practice was the order of the day. Besides this, diagnosis of malaria using the RDTs is quite handy.
We evaluated the immunodiagnostic technique synthesised in the US but produced by ‘Acon’ in china for its diagnostic efficacy and reliability. From the study, we found that with higher malaria density above 300 parasite per microliter (equivalent to two pluses (++), the kit was highly sensitive for diagnosis but below that level, the kit could hardly detect malaria parasites in blood samples.
In addition, the kit showed false positivity after malaria parasite clearance because the parasite antigen could still persist in the blood for about 24 hours after parasite clearance. The implication is that it may not be useful for children and immune deficient individuals because in such patients, low level malaria plasmodium in the blood (parasitaemia) could be the cause of their malaria. We therefore recommended the need for improvement in RDTs if it would be useful in children and in individuals with one form of impaired immunity or the other. The implication for medical practice is that appropriate interpretation is needed in clinical application of laboratory results based on RDTs in the management of patients (Odimayoet al 2004).
Mr Vice Chancellor Sir, microscopic examination of thick and thin blood film is the still the gold standard in the diagnosis of malaria. This I have devoted myself to teaching Medical Students and re-train other laboratory staff to do as much as possible. The Benue State Government recognized our commitment to this and commissioned my team for such trainings. We organized malaria diagnosis retraining programs for all laboratory staff in primary and secondary health care facilities in all local government in year 2010. Prevention as it is said, is better than cure. Among the roll back malaria initiatives is the use of Insecticide Treated Nets (ITNs).
The impregnation of pyrethrin into mosquito’s nets kills mosquitoes. It therefore was as if we have gotten to the end of mosquitoes which implies closeness to the end of the malaria scourge. What a wonder! Surprisingly, as months and years rolled by, there was no significant reduction in mosquitoes’ density. We were curious! What could be happening? We studied the use of ITNs in a semi urban community in Okpoga, Benue state, Nigeria and discovered that though over 85% of the populace were aware of its availability and over 80% have used and confirmed its efficacy; only 26% used it in the 6months preceding the study.
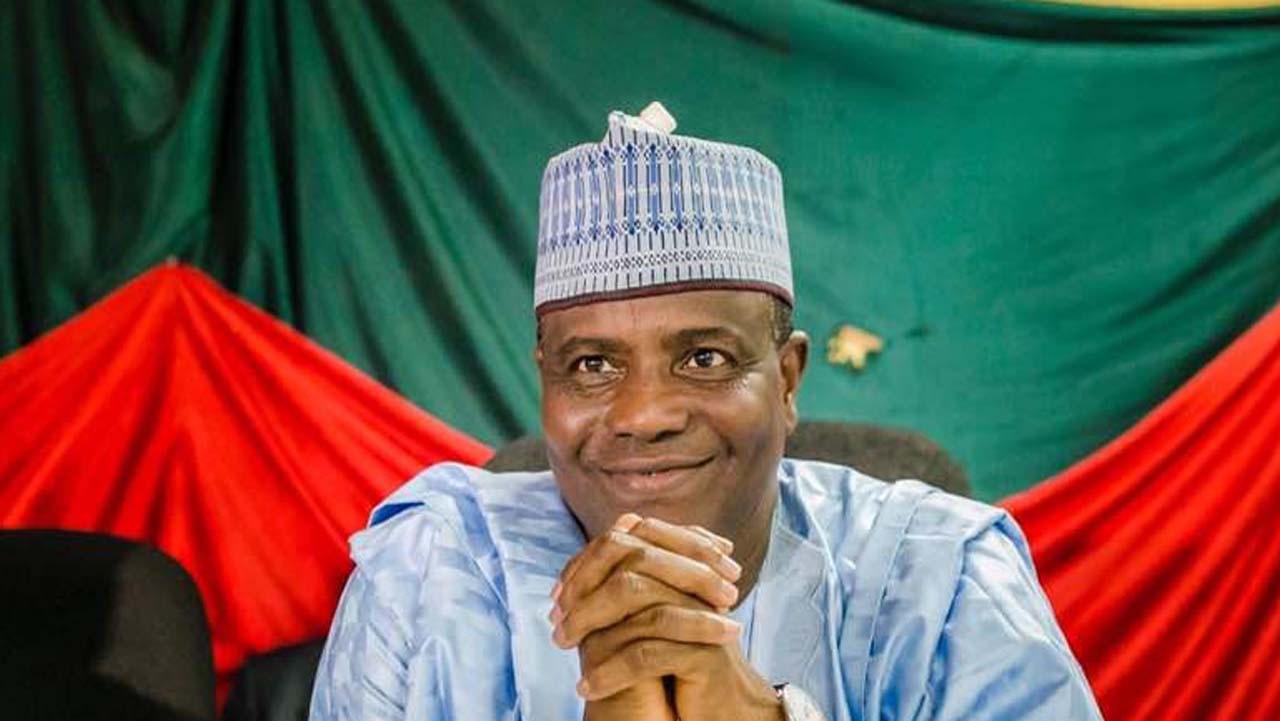
Odimayo is Professor of Microbial Pathology/Infectious Diseases delivered this inaugural lecture series 1 in Ondo, recently.