 The prevalence of cervical cancer in Nigeria requires concerted efforts in preventing the disease and deaths among the female population. Cervical cancer is the second leading cause of cancer-related deaths in females between ages 15 and 44 in Nigeria. Resource-limited settings such as Africa south of the Sahara where Nigeria belongs bears a disproportionate 84 per cent of the global burden of the disease.
The prevalence of cervical cancer in Nigeria requires concerted efforts in preventing the disease and deaths among the female population. Cervical cancer is the second leading cause of cancer-related deaths in females between ages 15 and 44 in Nigeria. Resource-limited settings such as Africa south of the Sahara where Nigeria belongs bears a disproportionate 84 per cent of the global burden of the disease.
This worrying statistic highlights substantial disparities in disadvantaged and underserved populations. Yet, luckily, cervical cancer is highly preventable through early and routinised screening to detect precancerous lesions. Evidence shows that incidence and death rates of cervical cancer have decreased in high-income countries due to early detection and treatment.
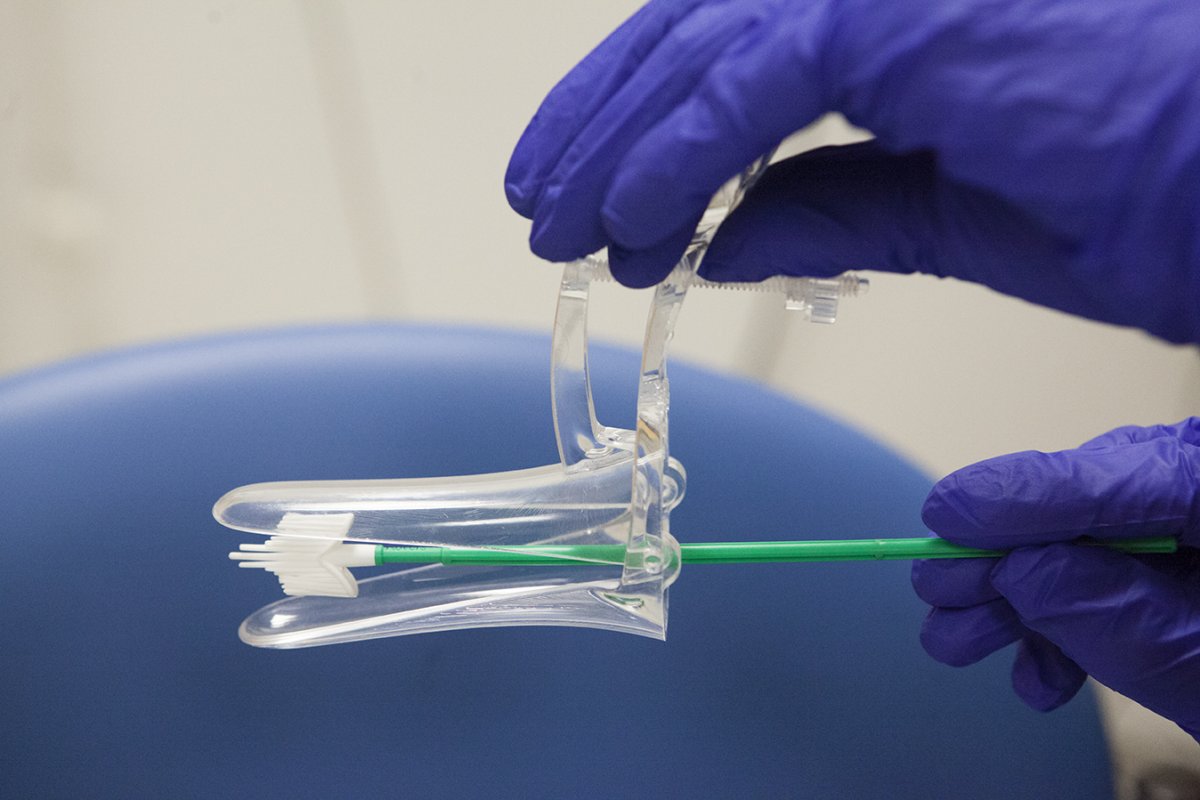
The high rates of cervical cancer cases and deaths in Nigeria present an opportunity for important engagement between public health, clinical health practice, and community-based organising. General screening guidelines stipulate pap testing for women aged 25–29 years every three years and pap and HPV testing every five years for women aged 30 to 65 years. Although countries such as Barbados, South Africa, and the United States begin at age 21. These significant strategies are key to fast-tracking WHO’s 2030 global target of ending cervical cancer as a public health threat.
Strategies to increasing screening rates involve improving cervical cancer prevention programs and expanding access to services. Cervical cancer screening data shows low screening rates of 1 to 10 in Nigerian women. Key findings on screening disparities indicate 84 per cent screening in women aged 30–49 years living in high-income countries compared to 9 per cent in lower-middle-income countries and 11 per cent in low-income countries.
Approaches to improving prevention include increasing education on cervical cancer and pap screening to urban and rural women, specifically on the importance of pap screening and early detection, causes and risks of cervical cancer, and screening locations.
Poor knowledge and information on the causative agent – the human papilloma virus (HPV) – and cervical cancer and screening are some of the factors that perpetuate this disturbing disparity in screening rates.
Evidence linking these factors to the low uptake of cervical cancer prevention services have been documented in numerous studies. However, knowledge alone may not instigate behavior change, but understanding the impact of culture to frame solutions.
Health communication researchers submit that cultural sensitivity to increasing knowledge and uptake of screening services can be impactful especially in close-knit communities such as in Nigeria that value family and interpersonal communication, and health information shared by family health decision makers and close relationship networks.
The influence of healthcare provider requested pap screening and support from social networks revealed in my recent study submitted for publication establish the need to strengthen and utilise interpersonal and group communication strategies to increasing knowledge and influencing screening behavior in Nigerian women.
It is strategic to disseminate information in a manner that aligns with the way community members typically receive and share health information.
As such, intervention approaches integrating women, men, clergy, and groups, alongside healthcare providers in educating and influencing women to screen, are promising. Relatedly, during screening, women’s preference of female providers collecting their pap samples should be recognised and conceded to.
Nonetheless, the solution to the worrying cervical cancer situation in Nigeria is many-sided, requiring manifold efforts by health advocates, health care providers, and community members. Increased media coverage on pap screening and other cervical cancer prevention information is another strategic tool.
Ample amounts of health information and coverage will communicate importance, thereby creating perceptions of high relevance and risk. People who perceive high susceptibility and severity are likely to adopt recommended health behaviors. Media coverage on cervical cancer prevention can be spearheaded by government, nonprofits, and news stakeholders.
This integrative approach through public education, interpersonal and group communication, and such other normative strategies embedded in culture offer a glimpse of how pap screening can be improved in Nigeria.
Dr Dadem is an Assistant Professor of Communication at Coker University, United States.






