The World Health Organization (WHO) has released a draft Global Strategic Preparedness and Response Plan (SPRP) for Mpox, covering the six-month period from September 2024 to February 2025.
The response plan, which stresses surveillance, research, equitable access to medical countermeasures, and community empowerment to respond to this global emergency, provides a framework for public health preparedness and response to the Mpox emergency.
READ ALSO:British rock legends, Oasis, announce worldwide reunion tour
According to the global health body, under the SPRP, the initial six-month operation will focus on controlling acute outbreaks of human-to-human transmission, with an estimated budget of US$135 million for international support to national Mpox responses.
Information released by the WHO indicates that the current draft, subject to Member State input, outlines the urgent actions needed at global, regional, and national levels.
It stated that the WHO Director-General determined that the Mpox upsurge was a public health emergency of international concern on August 14, 2024, given the detection and rapid spread of a new clade of Mpox in eastern Democratic Republic of the Congo, its detection in neighbouring countries that had not previously reported Mpox, and the potential for further spread within Africa and beyond.
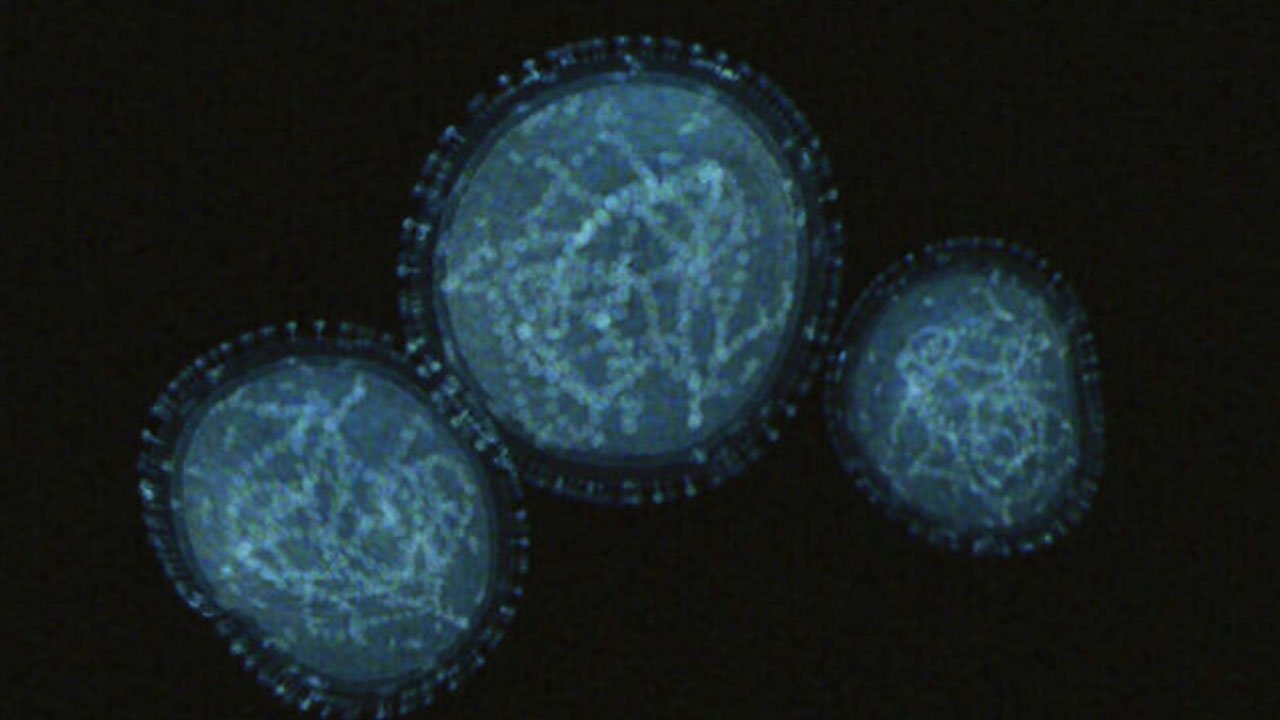
The WHO explained that Mpox, previously known as monkeypox, is a viral illness caused by the monkeypox virus, a species of the genus Orthopoxvirus. It added that there are two distinct clades of the virus: clade I (with subclades Ia and Ib) and clade II (with subclades IIa and IIb), noting that in 2022–2023, a global outbreak of Mpox was caused by the clade IIb strain.
READ ALSO:Nigerians react as minister seeks woman who shared mom’s mental health video
It noted that Mpox continues to be a threat today, and an upsurge of cases in the Democratic Republic of the Congo and other countries caused by clades Ia and Ib has raised concern.
Pointing out that there are vaccines for Mpox, the WHO advised that vaccination should be considered along with other public health interventions, warning that Mpox can be transmitted through close contact with someone who has the disease, with contaminated materials, or with infected animals.
The UN body re-emphasized that common symptoms of Mpox include a skin rash or mucosal lesions that can last 2–4 weeks, accompanied by fever, headache, muscle aches, back pain, low energy, and swollen lymph nodes.
WHO pointed out that during pregnancy, the virus may be passed to the foetus, or to the newborn during or after birth, while people with multiple sexual partners are at higher risk of acquiring Mpox.
“During pregnancy or birth, the virus may be passed to the baby. Contracting Mpox during pregnancy can be dangerous for the foetus or newborn infant and can lead to loss of the pregnancy, stillbirth, death of the newborn, or complications for the parent. Children, pregnant people, and people with weak immune systems, including those living with HIV that is not well controlled, are at higher risk for serious illness and death due to complications from Mpox,” it stated.
It noted that Mpox is treated with supportive care for symptoms such as pain and fever, with close attention to nutrition, hydration, skin care, prevention of secondary infections, and treatment of co-infections, including HIV where present.
READ ALSO:Paris Paralympics organisers announce two million tickets sold
According to the WHO, over 120 countries have reported Mpox between January 2022 and August 2024, with over 100,000 laboratory-confirmed cases reported and over 220 deaths among confirmed cases.
The WHO warned that stigma and discrimination for any disease are never acceptable, stressing that stigma linked to Mpox can undermine public health efforts or prolong a disease outbreak, as people may be more reluctant to come forward and seek care and treatment.
“For Mpox, stigma, discrimination, and racism have been particularly directed against communities initially most affected by the disease, namely men who have sex with men, trans people, and gender-diverse communities.”
The WHO advised that to contain the spread of Mpox to others, people with Mpox should isolate at home following guidance from their health care provider, or in hospital if needed, for the duration of the infectious period (from onset of symptoms until lesions have healed and scabs fall off).
“Covering lesions and wearing a well-fitting mask when in the presence of others may help prevent spread. Using condoms during sex will help reduce the risk of getting Mpox but will not prevent spread from skin-to-skin or mouth-to-skin contact. If having sex, use condoms as a precaution for 12 weeks (about 3 months) after you have recovered.”
“Taking a break from sexual activity with new partners during periods of increased transmission can reduce the risk of getting Mpox. Those who have had contact with someone with Mpox should monitor for signs and symptoms for 21 days (3 weeks) and take precautions such as avoiding sexual activity during this period,” it added.
The WHO also urged health workers to follow infection prevention and control measures to protect themselves while caring for patients with Mpox by wearing appropriate personal protective equipment (PPE) such as gloves, gowns, eye protection, and respirators, and adhering to protocols for safely swabbing lesions for diagnostic testing and handling sharp objects such as needles.
According to the organisation, the preferred laboratory test for Mpox is the detection of viral DNA by polymerase chain reaction (PCR), and the best diagnostic specimens are taken directly from the rash – skin, fluid, or crusts – collected by vigorous swabbing.
However, in the absence of skin lesions, testing can be done using swabs from the throat or anus, while testing blood is not recommended.
The organisation said that HIV testing should be offered to adults with Mpox and children as appropriate, while individuals with HIV and Mpox should continue taking their antiretroviral therapy (ART). ART should be initiated within seven days of diagnosis of HIV.
“Mpox is an infectious disease that can cause a painful rash, enlarged lymph nodes, fever, headache, muscle ache, back pain, and low energy. Most people fully recover, but some get very sick. Mpox is caused by the monkeypox virus (MPXV). It is an enveloped double-stranded DNA virus of the Orthopoxvirus genus in the Poxviridae family, which includes variola, cowpox, vaccinia, and other viruses. There are two distinct clades of the virus: clade I (with subclades Ia and Ib) and clade II (with subclades IIa and IIb).
“A global outbreak of clade IIb began in 2022 and continues to this day, including in some African countries. There are also growing outbreaks of clades Ia and Ib affecting the Democratic Republic of the Congo and other countries in Africa. As of August 2024, clade Ib has also been detected beyond Africa. The natural reservoir of the virus is unknown, but various small mammals such as squirrels and monkeys are susceptible,” it added.
The WHO explained that Mpox spreads from person to person mainly through close contact with someone who has Mpox, including members of a household. Close contact includes skin-to-skin (such as touching or sex) and mouth-to-mouth or mouth-to-skin contact (such as kissing), and it can also include being face-to-face with someone who has Mpox (such as talking or breathing close to one another, which can generate infectious respiratory particles).
It added that people can also contract Mpox from contaminated objects such as clothing or linen, through needle injuries in health care, or in community settings such as tattoo parlours.
Animal-to-human transmission of Mpox occurs from infected animals to humans through bites or scratches, or during activities such as hunting, skinning, trapping, cooking, playing with carcasses, or eating animals. The animal reservoir of the monkeypox virus remains unknown, and further studies are underway.
More research is needed on how Mpox spreads during outbreaks in different settings and under different conditions.
Regarding the signs and symptoms of the disease, the WHO observed that Mpox causes signs and symptoms which usually begin within a week but can start 1–21 days after exposure. Symptoms typically last 2–4 weeks but may last longer in someone with a weakened immune system.
The WHO noted that it is working with Member States and partners to prevent and respond to outbreaks of Mpox, including coordinating research on vaccines and treatments, strengthening country health systems, and working to facilitate equitable access to vaccines, therapeutics, diagnostics, and other tools.
WHO Director-General Dr. Tedros Adhanom Ghebreyesus has declared Mpox a public health emergency of international concern (PHEIC) twice, the first time in May 2022 and the second time in August 2024.