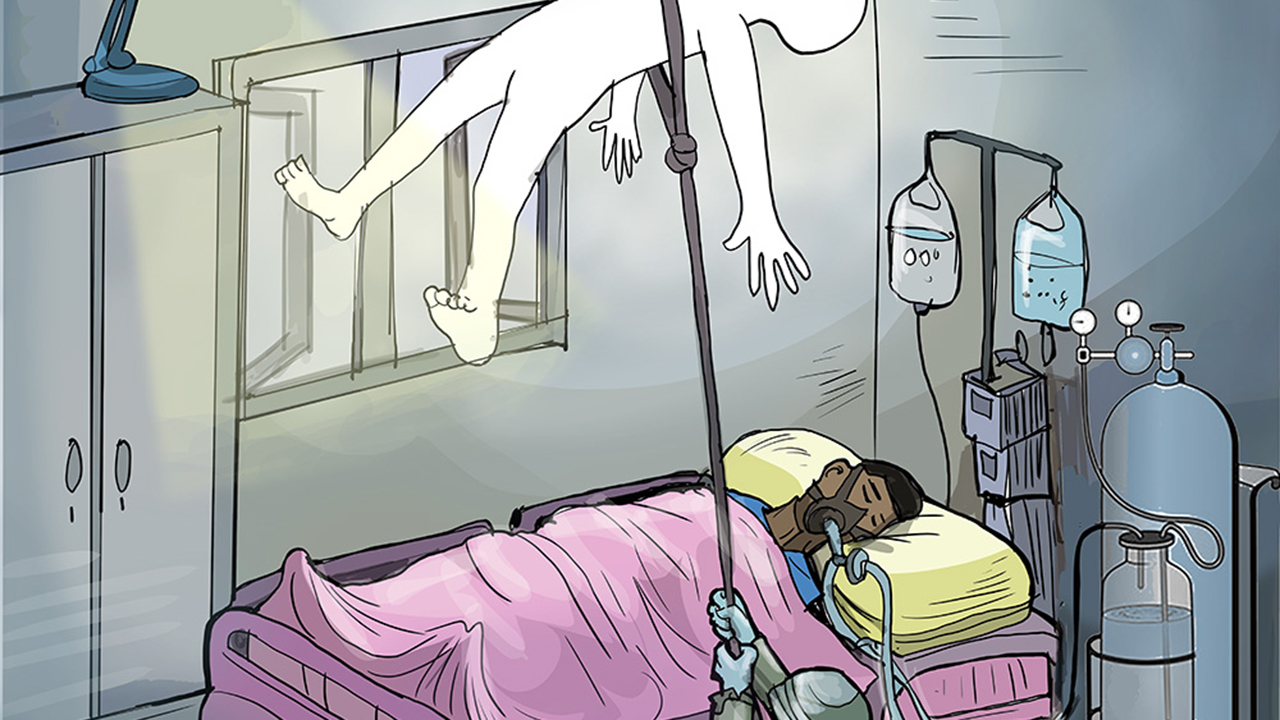
 For over three months, Nigeria’s premier teaching hospital, the University College Hospital (UCH), Ibadan, grappled with an unprecedented power crisis that disrupted surgeries, paralysed diagnostic services, and turned the once-revered facility into a dark abyss. Like an epidemic, poor energy access also plagued some other tertiary health facilities, leading to the untimely and avoidable death of many poor Nigerians, who are at the intersection of energy poverty, a high electricity tariff regime, and a frail health sector, whose underbelly is putrefying. WALIAT MUSA and IJEOMA NWANOSIKE write that the government must demonstrate its commitment to critical social services beginning with an end to the needless death of Nigerians in life-saving facilities owing to poor power access.
For over three months, Nigeria’s premier teaching hospital, the University College Hospital (UCH), Ibadan, grappled with an unprecedented power crisis that disrupted surgeries, paralysed diagnostic services, and turned the once-revered facility into a dark abyss. Like an epidemic, poor energy access also plagued some other tertiary health facilities, leading to the untimely and avoidable death of many poor Nigerians, who are at the intersection of energy poverty, a high electricity tariff regime, and a frail health sector, whose underbelly is putrefying. WALIAT MUSA and IJEOMA NWANOSIKE write that the government must demonstrate its commitment to critical social services beginning with an end to the needless death of Nigerians in life-saving facilities owing to poor power access.
Ezinne Nwandu, a middle-aged food vendor residing in Lagos State, was admitted to a private hospital due to a severe health condition. As days passed by without any sign of improvement, her worried family requested and obtained a referral that moved her to the Lagos University Teaching Hospital (LUTH).
Within a few days at LUTH, Nwandu showed significant improvement, bringing relief to her family, especially her husband, despite the high, daily costs of medication and other essentials.
However, her recovery journey suffered a major setback when the hospital’s public power supply was suddenly disconnected. The power outage halted crucial tests and treatments that relied on electricity-powered machines.
Concerned about the situation and the mounting medical bills, the Nwandus withdrew her from the hospital and relied solely on prescribed medications while hoping for a miracle that would aid her survival. Unfortunately, just three days after she left the hospital, she passed away.
When she opened up about the growing difficulties patients face due to inconsistent power supply at the University College Hospital (UCH), Ibadan, Oyo State, Adeola Hamzat, a relative of a patient that was admitted amidst the niggling power crisis, explained that relatives of some critically ill patients are usually flustered when they need to run critical medical tests, especially when the hospital only runs its power generating for about 30 minutes before switching it off, causing significant disruption to services.
Adeola, who was particularly startled when told at a critical time that a simple urine test could not be conducted at the hospital, was later directed to Mokola, a location far away from the UCH, to carry out the test.
“The situation has never been this bad because I once put to bed here, and there was always a power supply then. So, why all this?” A frustrated Adeola lamented.
Miss Rebecca Odeyemi, experienced firsthand, the thin line between life and death when her parent recently fell ill. According to her, many people are now hesitant when it comes to seeking medicare at the UCH due to fears that their conditions might worsen. She added that those who still relied on the hospital had to do so at an additional cost, and with significant effort.
The late Nwandu has sadly become part of the data emanating from Nigeria when cases of needless deaths are being tabulated, and cases like this are legion.
Without a doubt, frequent electricity disconnections plaguing tertiary hospitals across the country, contribute effectively to the ballooning death toll recorded in these facilities that have been overwhelmed by an energy crisis.
LUTH opened the floodgate of sad tales emanating from these hospitals, then followed by the UCH, in Ibadan, and several others, where poor and middle-class patients have continued to suffer in silence.
For over three months, the UCH – Nigeria’s premier teaching hospital was engulfed in a severe power crisis, which not only paralysed critical operations, ranging from life-saving surgeries to essential diagnostic services but also revealed the weak underbelly of the country’s frail health care system and the pathetic state of the country’s power supply.
Over the years, the UCH, a once-thriving hub for medical excellence has evolved into a symbol of Nigeria’s faltering infrastructure, and administrative shortcomings.
What began as a debt dispute between the hospital and the Ibadan Electricity Distribution Company (IBEDC) suddenly escalated into a national embarrassment, drawing widespread criticism.
These persistent electricity outages, which span over 100 days in some instances, have brought critical healthcare services to a standstill, risking patients’ lives and straining hospital operations.
As the crisis at the UCH festers, LUTH patients last year endured a prolonged blackout, which disrupted services, leaving patients and medical staff in dire straits as surgeries were suspended, and medical interventions requiring stable power supply were delayed in what was a grim reminder of how the interplay between rampant power failures and sub-optimal healthcare delivery can have catastrophic consequences.
The Guardian gathered that while the lack of essential services has resulted in the death of many patients in these teaching hospitals, the deceased in some morgues were not spared the dilemma as bodies were hastily evacuated for burial before they started decomposing.
A wave of electricity crazy bills, disconnections from national grid
LIKE most Nigerian homes and institutions, the health sector has had to contend with poor power access occasioned by recurring grid collapses, and rising electricity tariffs, which translate into hefty electricity bills. Prolonged blackouts occasioned by disconnections by distribution companies gradually turned into a nightmare for patients and their families.
As of the end of 2024, dangling on the necks of several teaching hospitals in the country were mounting electricity debts, which threatened effective service delivery. For instance, the N495 million debt that accrued to the UCH led to repeated disconnections by the Ibadan Electricity Distribution Company (IBEDC).
Similarly, the EKO Electricity Distribution Company (EKEDC) had earlier knocked off LUTH from the National Grid over an outstanding N275 million bill. In March 2024, LUTH, which relied on its power-generating plant for about seven years, disclosed that the rising electricity costs had become unsustainable for the hospital’s management, prompting a switch to Eko Disco. However, by June 2024, Eko Electricity Distribution Company (EKEDC) disconnected both the hospital and the College of Medicine over an outstanding debt of N252 million.
While the hospital claimed minimal disruption, as it relied on backup generators and inverters to maintain operations, The Guardian found out that the situation at the College of Medicine was worse. Students, who were frustrated by the prolonged outages, took to social media to voice their grievances and thereafter protested against the persistent power crisis.
In Enugu State, the Chukwuemeka Odumegwu Ojukwu University Teaching Hospital (COOUTH), Amaku-Awka, was left without electricity for two weeks after the Enugu Electricity Distribution Company (EEDC) issued an April 2024 bill of N19.8 million.
Up North, the Aminu Kano Teaching Hospital (AKTH) suffered power disruptions due to an unexpected N30 million debt imposed by the Kano Electricity Distribution Company (KEDCO), and in May 2024, AKTH received another staggering electricity bill of N119 million.
This crisis has severely impacted the system, with devastating consequences for patients. Experts revealed that many have faced delays in tests and treatments, cancellations or postponements of surgeries, and an overwhelming financial burden.
Painting a horrible scene that is becoming commonplace in some teaching hospitals across the country, a pediatrician, who was on-call duty, recently recalled a particular night that almost claimed the life of a pregnant woman.
Although his unit had rechargeable lamps for illumination, which could not last the night, he expressed frustration at having to execute ward rounds using his mobile phone’s flashlight, and even administering intravenous (IV) medications in dimly lit atmospheres,” he said.
Pass the cost to hapless patients
LAST November, the management of Federal Medical Centre (FMC) Asaba, Delta State, raised concerns over the growing financial strain caused by the new electricity tariff, and the constant need to rely on power generating sets due to frequent power outages.
The Chief Medical Director (CMD) of the hospital, Dr Victor Osiatuma, told The Guardian that this had led to an inevitable 20 per cent increase in costs, which was being passed on to patients seeking medications, or routine services to sustain hospital operations.
A similar scenario also played out at General Hospital, Isolo, where a source disclosed that the electricity tariff hike was already affecting patients, albeit slightly.
According to him, routine procedures such as blood screening were no longer financially viable for the hospital to run, while the cost of power generation also skyrocketed, consuming nearly 12 times its previous budget. This, the source noted, severely strained the hospital’s overhead allocation, making it increasingly difficult to maintain affordable healthcare services.
To a reasonable extent, the power crisis rocking teaching hospitals can be described as a direct consequence of broader systemic issues within the power sector. One of which is the electricity subsidy removal by the Federal Government, and the migration of customers, including large institutions like hospitals to Band A electricity tariff, which ties into the subsidy framework within the country’s power sector.
Subsidies are intended to bridge the gap between the cost of electricity production and the tariffs charged to consumers. However, inefficiencies and financial shortfalls have led to liquidity crises for electricity distribution companies (DisCos), compelling them to take drastic measures, including, but not limited to disconnecting non-paying institutions.
Previously, subsidies cushioned the financial burden of electricity tariffs for public institutions. With the removal of these subsidies and the enforced migration to Band A, which mandates higher tariff rates in exchange for a more stable power supply, hospitals are now grappling with skyrocketing energy costs.
In November, the steep costs associated with the new tariff structure made it impossible for FMC Ebute-Metta, Lagos, to upgrade to Band A. According to the hospital management, the power supply under Band B remained highly unreliable, with the facility receiving only about three hours of electricity on a good day.
Speaking to The Guardian, hospital officials described the situation as unsustainable, as they are forced to rely heavily on diesel power generating sets, which consume an estimated 80,000 to 100,000 litres each month to keep operations running.
A similar heavy reliance on power plants was reported at the University of Ilorin Teaching Hospital (UITH) in July 2024, as the facility struggled with months of unstable power supply.
The chairman of the Association of Resident Doctors (ARD) at UITH, Dr Yusuf Mohammed, disclosed that the inadequate electricity supply resulted in postponed surgeries and reduced clinic hours, severely affecting patients’ care.
Due to the migration to Band A, Ahmadu Bello University Teaching Hospital (ABUTH) pays over N70 million monthly; Aminu Kano Teaching Hospital pays over N100 million per month; Abubakar Tafawa Balewa University Teaching Hospital, Bauchi (ATBUTH) pays about N50 million monthly; Jos University Teaching Hospital (JUTH) coughs out about N30 million, and University of Nigeria Teaching Hospital (UNTH) pays about N50 million monthly for electricity.
The Federal Government has been subsidising electricity tariffs to cover the gap between production costs and consumer tariff charges. In the third quarter of 2024, the government incurred a subsidy obligation of N464.12 billion representing 54.71 per cent of the total Nigerian Bulk Electricity Trading (NBET) invoice, up from N380.06 billion in the second quarter of 2024.
However, The Guardian’s check revealed that, at the currently allowed tariffs, the market is projected to face a tariff shortfall of N2.36 trillion in 2025, with indications that no provision has been made for it in the proposed budget for the year.
Further checks revealed that tariffs need to be cost-reflective to ensure the sustainability of Generation Companies (GenCos). The current end-user tariffs have remained frozen since December 2022 for Bands B to E and July 2024 for Band A, limiting the ability of Distribution Companies (DisCos) to settle only 40 per cent of GenCos’ monthly invoices.
Despite these substantial subsidies, challenges remain. For instance, a 2021 World Bank report revealed that 59.5 per cent of tariff subsidies benefit the richest 20 per cent of households, while only 1.5 per cent reaches the poorest 20 per cent, highlighting a pro-rich bias in subsidy distribution.
Public hospitals or morgues?
REFLECTING the concerns of many patients and their families, especially how power crisis undermines patients’ safety and quality medicare, the Unit Head of the Endocrinology, Diabetes, and Metabolism Division at LUTH, Prof. Olufemi Fasanmade described the persistent power outages in teaching hospitals as a “dangerous” crisis.
He warned that these disruptions not only undermine the quality of medical care but also pose serious risks to patients’ safety as a steady power supply is essential for hospitals to function effectively.
He expressed deep concern over the power cuts at UCH, noting that the transition to Band A accompanied by significantly higher electricity tariffs had drastically increased hospital expenditures with little prior notice. This sudden financial strain, he explained, left hospitals unable to sustain payments, leading to frequent disconnections that directly threaten patient care.
Fasanmade, who highlighted the severe consequences of power outages including delays in medical tests, poor patient accommodations, and the cancellation or postponement of surgeries, stressed that critical procedures such as MRIs, X-rays, and surgeries were being severely affected due to the unreliable power supply.
The unit head further underscored the gravity of the crisis, emphasising that a teaching hospital of UCH’s magnitude cannot function effectively without a constant power supply.
He criticised both the government and the hospital’s management for failing to take proactive measures to address the situation. According to him, investments in alternative energy sources such as solar panels and independent power plants could have mitigated the crisis and reduced dependence on the national grid.
Fasanmade called on the government to take urgent action, not just for the UCH but for other hospitals facing similar power supply challenges as many hospitals were either plunged into darkness or receiving only a few hours of electricity daily, forcing them to rely heavily on diesel-powered generators, a costly and environmentally harmful alternative.
“Patients are the ones who are losing big time as far as this issue is concerned. Nobody may want to go into the specifics, but generally, just bear in mind that operations are delayed, postponed, or cancelled,” he noted.
An expert in anaesthesia and intensive care, Dr Akintade Adegboyega, said that the consequences of erratic electricity supply are deadly as medical devices such as Magnetic Resonance Imaging (MRI) machines, incubators for newborns, and oxygen supply systems all require constant electricity.
“An MRI machine cannot be turned off once it’s powered on. If the power goes out, specialists from the manufacturer must come to restart it, which is both costly and time-consuming. Also, when performing surgery, the monitors, suction machines, and life-support equipment all rely on continuous power, and if they stop working, patients can die in minutes.”
Adegboyega said the reliance on backup generators is costly and unsustainable as one major hospital in Lagos reportedly spends close to N300 million per month just on diesel, adding that the cost is passed on to patients, making healthcare 30 per cent to 40 per cent more expensive than it should be.
The National Coordinator of All Electricity Consumers Protection Forum (AECPF), Adeola Samuel-Ilori, blamed successive governments’ failure to fix the power sector for Nigeria’s economic crisis, including the mass exodus of medical personnel abroad.
He noted that, like industries, hospitals also rely on power, stressing that the crisis impacts the medical sector more, including the pharmaceutical industry, which is integral to healthcare. He added that it would be unwise for surgeons to operate without ensuring a reliable power source, whether from the grid, generators, or renewable energy.
“Why do you think our leaders and the nouveau riche choose to go abroad for medical tourism, rather than patronise any medical facility here for checkups and minor surgeries? It’s mainly because of the non-availability of power supply and moribund equipment that are predominantly in our public and government-owned hospitals and medical institutions. Do you think anyone with his or her family in that hospital in the last three months would still leave their loved ones there if they have the wherewithal of the chance to go abroad?” he explained.
Innovating to keep hope alive
TO address power supply challenges, some teaching hospitals, such as the University of Maiduguri Teaching Hospital, with a 12MW capacity, and the University of Calabar Teaching Hospital with a 7MW capacity, have adopted captive power generation approved by the NERC, enabling them to produce their electricity.
The Federal Government has also listed both the UCH and the University of Ibadan as beneficiaries of a 50-megawatt solar mini-grid, which will be completed on or before June this year. The projects fall under the second phase of the Energising Education Programme (EEP) of the Rural Electrification Agency (REA).
Apart from UNICAL and UNIMAID, similar interventions that have been successfully implemented are at the University of Abuja, the Federal University of Agriculture Abeokuta, and the Nigerian Defense Academy, Kaduna.
While the power supply crisis affecting teaching hospitals underscores the complex interplay between healthcare funding, energy policy, and subsidy management, guaranteeing stable power supply is not merely an operational requirement, but an essential factor in providing quality healthcare services to Nigerians.
The implications of such power failures go beyond mere inconvenience as reliable electricity is the backbone of life-saving services. From powering surgical equipment to maintaining cold-chain storage for essential vaccines and medications, electricity is as vital as any medical tool.
The Mission 300 initiative, which the Federal Government recently signed up to presents a potential solution to the country’s lingering electricity challenge as it aims to accelerate electrification by integrating grid expansions with decentralised renewable energy solutions, such as mini-grids and stand-alone solar home systems. These innovations are particularly beneficial for reaching vulnerable and remote areas where extending traditional grid infrastructure remains impractical.
Additionally, the initiative emphasises investments in power generation, transmission, regional interconnection, and sector reforms to ensure a reliable, affordable, and sustainable electricity supply.
Be that as it may, the growing public outrage and media attention that the UCH Ibadan power saga generated forced the Federal Government to step in to address the situation. After several high-level meetings, including negotiations with IBEDC, the Minister of Power, Adebayo Adelabu announced plans to settle part of the hospital’s debt with the restoration of power supply.
Describing the blackout as a national embarrassment, not just for the hospital or the distribution company, but also for the Federal Government, Adelabu noted that the power crisis remains a shameful situation for a premier institution and underscores broader issues in Nigeria’s power sector. He attributed the hospital’s huge debt to several factors, including sharp practices, unseparated accounts, dilapidated infrastructure, and ageing equipment.
“The Federal Government desires to see that all institutions are electrified, however a proper energy budget must be done by all institutions and submitted to the parent body, the Federal Ministry of Health. Henceforth, each of the major consumers will be responsible for the payment of their electricity bills as against the previous practice of lumping bills,” Adelabu said.
As power gets gradually restored and debts negotiated, questions still linger about the future of teaching hospitals, and the likelihood of the lingering crises serving as a turning point for better resource management and infrastructure investment. For electricity market analyst, Lanre Elatuyi, migrating health institutions to Band A benefits these public facilities, provided the agreed service hours are met. He further told The Guardian that while subsidies can support institutions like healthcare centres their sustainability depends on government funding. He also emphasised the importance of energy efficiency in ensuring that these facilities maximise the benefits of the subsidy.
“The onus is on the part of public institutions to pay their bills regularly because they do have budgets for utilities. So, it shouldn’t be hard to pay their bills. It is also advisable that they conduct a proper load study and also do an energy audit to see where improvements can be made in terms of being energy efficient. It is also concerning that some of these public institutions will rather opt to buy diesel to fuel generators than pay electricity bills for personal gains,” he said.
He emphasised that DisCos must avoid estimated billing and ensure that electricity is supplied at the correct voltage to make power supply reliable and beneficial to consumers.






