 Moyosore Salami examines what andropause entails, its symptoms, and its impact on daily life, on a condition that is frequently underrecognised and undertreated.
Moyosore Salami examines what andropause entails, its symptoms, and its impact on daily life, on a condition that is frequently underrecognised and undertreated.
As society becomes increasingly aware of menopause and its effects on women, another age-related condition affecting men is gradually gaining attention: andropause. Often overshadowed by its female counterpart, menopause, sometimes, referred to as male menopause or Partial Androgen Deficiency of the Aging Male (PADAM), is a significant health issue impacting many men as they age.
Andropause is characterised by a decline in testosterone levels, the male hormone crucial for libido, energy, and overall vitality. Unlike menopause, which is marked by the clear cessation of menstrual cycles, andropause lacks a definitive marker, making it less recognized and often overlooked. The condition typically begins in middle age like 48 and becomes more pronounced as men reach their 60s and 70s, with testosterone levels often falling by up to 35 per cent compared to younger men.
The symptoms can range from diminished sexual desire and energy levels to mood disturbances and difficulty concentrating. These changes often lead to excessive fatigue, a general disinterest in activities once enjoyed, and a significant drop in the overall quality of life.
Despite its prevalence, exact figures on how many men experience it are elusive, partly due to the condition being frequently underreported and misattributed to other health issues.
Differentiating andropause from normal aging can be challenging, as many symptoms overlap. Diagnosis generally occurs after ruling out other conditions and confirming low testosterone levels.
While it can begin at various ages, its effects are usually more noticeable in older men. Unlike menopause, the onset of andropause does not follow a specific timeline, varying widely among individuals.
It is linked to several health concerns, including osteoporosis and cardiovascular issues, as testosterone plays a role in maintaining muscle mass and bone density.
However, these conditions could impact fertility and sexual function, as it’s reduces hormone level that affects libido and sperm production.
According to experts, the mental and emotional toll of andropause can be profound. Struggles with sexual function could lead to relationship strains and associated mental health issues, including depression.
Addressing these symptoms often involves a combination of lifestyle changes such as improved diet, regular exercise, and moderation in alcohol consumption, as well as medical treatments.
Medical experts emphasised the importance of early diagnosis and treatment. Testosterone replacement therapy (TRT) is one option for managing the symptoms, available in various forms, including tablets, patches, and injections. However, TRT is not without risks. Unregulated testosterone therapy can exacerbate conditions like prostate cancer or lead to aggressive behavior, making it crucial for treatment to be tailored to each individual’s needs and monitored closely for potential side effects.
A medical expert, Toluwanimi Adeyanju explained that unlike menopause in women, which is marked by the clear cessation of menstrual cycles, andropause lacks a definitive onset. This ambiguity, coupled with the gradual decline in testosterone, makes it harder to recognise and diagnose.
“The decline in testosterone doesn’t occur as rapidly as the drop in estrogen during menopause, so the symptoms can be less noticeable but no less significant, these symptoms can include decreased lean muscle mass, increased body fat, erectile dysfunction, depression, and fatigue, among others.”
Adeyanju emphasized that while not all men with reduced testosterone levels experience these symptoms, those who do often find their daily lives significantly impacted.
One critical area Adeyanju highlighted is mental health. Depression, a common symptom, can deeply affect a man’s outlook on life, leading to social withdrawal and strained relationships, particularly when sexual function is compromised.
Additionally, the physical decline associated with andropause can increase the risk of falls and fractures, potentially leading to a loss of independence and the need for assisted care, he noted.
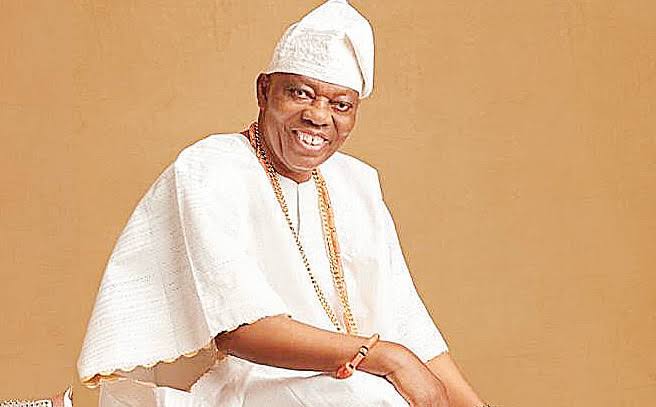
An endocrinologist, Dr Femi Ojo, explained the importance of breaking the silence around andropause.
“Andropause is a natural part of aging, but because the symptoms develop gradually, many men don’t recognise them as part of a hormonal change. They may attribute these changes to stress, aging, or other factors, without realising that their testosterone levels might be the underlying cause.”
Ojo added that understanding andropause as a normal part of aging can encourage men to seek treatment and support, helping them maintain their health, vitality, and well-being as they age.
“Breaking the silence around andropause is key; when men understand that what they are experiencing is a normal part of aging, they are more likely to seek treatment and support. By addressing andropause proactively, we can help men maintain their health, vitality, and well-being as they age.”
A consultant urologist, Dr Funmilayo Ajayi, told The Guardian that many men experience a significant drop in their quality of life during this phase.
“Men undergoing andropause often report feeling less energetic and more irritable. They may also struggle with sleep disturbances and cognitive issues, such as memory loss or difficulty concentrating.”
On the challenges of andropause, the doctor said these symptoms can be particularly challenging for men who are still in their working years or are dealing with other life stressors, such as caring for aging parents or coping with career changes.
She noted that the stigma surrounding male vulnerability often prevents men from seeking help, exacerbating their struggles.
“Men are often reluctant to discuss these issues, even with their doctors, due to societal expectations around masculinity and strength.”
A geriatric specialist, Dr Abimbola Olanrewaju, emphasized the need for greater awareness and intervention in addressing andropause.
“We need to raise awareness among both men and healthcare providers about the reality. Early diagnosis and intervention can significantly improve quality of life. This might include hormone replacement therapy (HRT), lifestyle modifications like diet and exercise, or counseling to address emotional and psychological symptoms.”
However, Olanrewaju cautioned that testosterone replacement therapy should not be viewed as a one-size-fits-all solution.
“It is essential to tailor treatment to each individual’s needs and to monitor patients closely for potential side effects, such as an increased risk of cardiovascular disease or prostate issues.”
A psychologist, Dr. Sarah Adeyemi, also noted the psychological impact of andropause, emphasizing the need for mental health support.
“The emotional symptoms of andropause, such as mood swings and depression, can be just as debilitating as the physical symptoms. It is crucial that men have access to mental health support during this transition. Cognitive-behavioral therapy (CBT) and other therapeutic interventions can be incredibly beneficial in helping men cope with these changes.”
Given the significant impact andropause can have on men’s health, medical experts advised that more needs to be done to bring this issue to the forefront. Public health campaigns, routine screening for testosterone levels in aging men, and open discussions in medical consultations can help demystify andropause and encourage men to seek the help they need.