 From dearth of hospitals and mental health professionals to lack of basic amenities and poor funding, it is glaring that psychiatric care in Nigeria is in dire strait, also as the number of mental cases has spiked by over 200 per cent in the last few months. In 2020, the Nigerian Medical Association (NMA) revealed that there were only 350 psychiatrists for Nigeria’s population of about 200 million people. Now, with brain drain and a lot of experts relocating abroad for greener pastures, it is expected that the number of psychiatrists to cater to the same population would have been far less than 350 with some consequences for the country, GBENGA AKINFENWA writes.
From dearth of hospitals and mental health professionals to lack of basic amenities and poor funding, it is glaring that psychiatric care in Nigeria is in dire strait, also as the number of mental cases has spiked by over 200 per cent in the last few months. In 2020, the Nigerian Medical Association (NMA) revealed that there were only 350 psychiatrists for Nigeria’s population of about 200 million people. Now, with brain drain and a lot of experts relocating abroad for greener pastures, it is expected that the number of psychiatrists to cater to the same population would have been far less than 350 with some consequences for the country, GBENGA AKINFENWA writes.
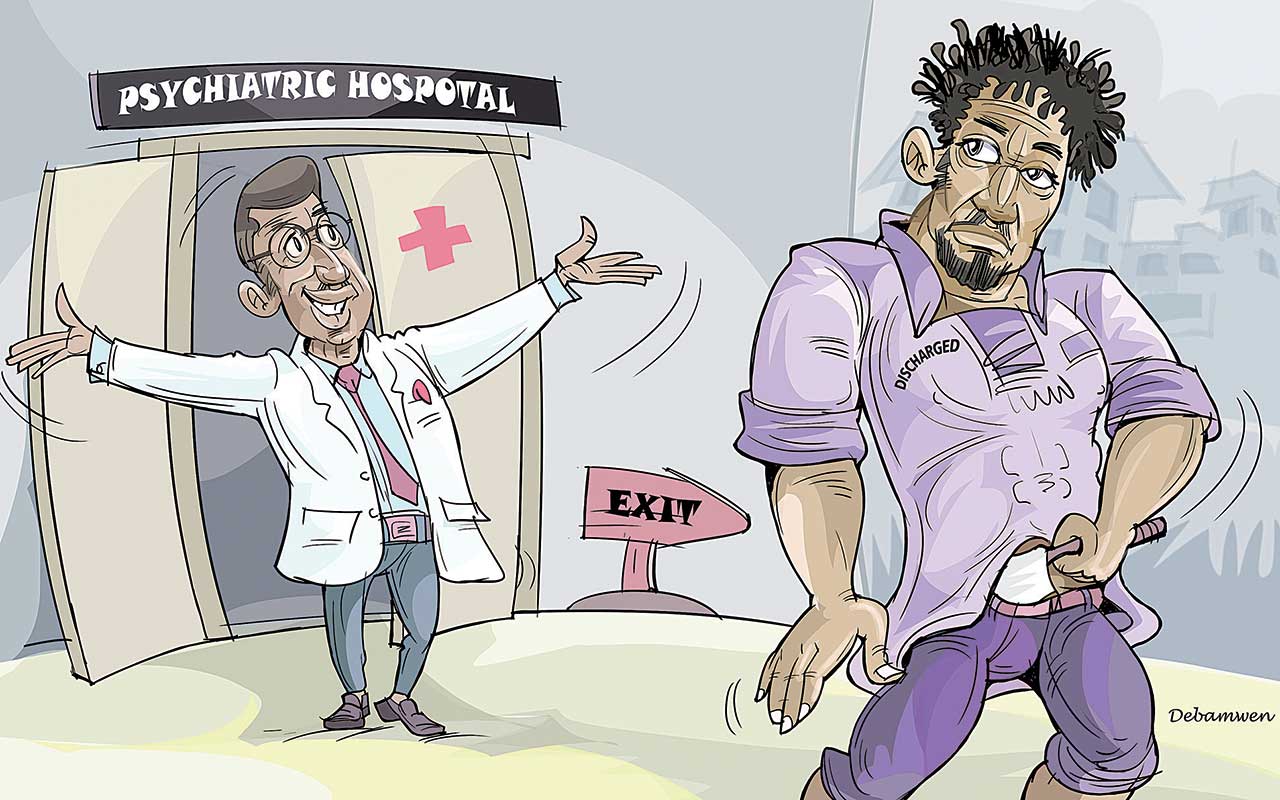
On January 1, 2021, a middle-aged man, Peter Akinjogun, a psychiatric patient in Ogun State, was discharged on the claim that he had been certified sane and could return to the society to mingle with other people.
To his family, his return that morning was like a New Year gift, as the man had suffered mental disorder since 2017, and had been in and out of hospitals within Ogun and Lagos states.
It was joy unlimited because he reunited with the family at a time when everyone came home to celebrate the Christmas festivity with their aged parents. But the happiness that trailed the discharge of the patient was cut-short a few hours after his return. Around 5:30pm that day, Peter stabbed his step brother, a 42-year-old man, Femi Akinjogun, to death after a little misunderstanding.
The tragedy, which shook the entire Salami Ojerinde and adjoining streets at Powerline in Agbado-OkeAro area of Ifo Local Council, Ogun State, left a major scar in the family, and till date, the mare still haunts the family.
The incident occurred during the slaughtering of a ram to celebrate the New Year. Femi, who lived in the family house with his two sons and a pregnant wife, had sought the assistance of Peter in butchering the ram. Peter was not happy with the request and a minor altercation followed. In the process, Peter picked up a knife and stabbed his brother in the neck in the presence of everybody, including his wife, who was pregnant. Femi was rushed to the hospital, but he couldn’t make it, as he died on the way.
The incident later became a matter of serious concern, as Nigerians, especially friends of the deceased raised questions on why and how a psychiatric patient would be certified fit and discharged when he was still mentally unstable.
The incident is one of the many tragic cases associated with psychiatric patients. There are reports that many similar cases have either been under-reported or swept under the carpet, making it difficult to address the preventable tragedies.
A victim of mental patient’s brutality, Ruth Idowu, who shared her bitter experience with The Guardian, said the incident almost claimed her life. Still, the attack by a madman, which occurred when Idowu was 17 years old, left her permanently disfigured. She said the incident was enough to force her to commit suicide, but owing to ‘will-power’ and the drive to succeed, she kept on struggling with life. The attack led to the cutting of her two wrists.
 “On October 2, 2010, while I was assisting my mother in her restaurant at Oja-Odan, Yewa North Local Council, Ogun State, I stood at the entrance inward the restaurant. Suddenly, I noticed someone approaching the doorway, behold, it was a madman, holding a machete and was aiming straight for my head.” Panic-stricken, she took to her heels to escape from the impending doom, but fell in the process. The man caught up with her and began to strike her with the machete.
“On October 2, 2010, while I was assisting my mother in her restaurant at Oja-Odan, Yewa North Local Council, Ogun State, I stood at the entrance inward the restaurant. Suddenly, I noticed someone approaching the doorway, behold, it was a madman, holding a machete and was aiming straight for my head.” Panic-stricken, she took to her heels to escape from the impending doom, but fell in the process. The man caught up with her and began to strike her with the machete.
“To prevent him from cutting off my head and neck, I used my two hands as defence and in the process my two wrists were completely cut off. By the time sympathisers rushed out to rescue me, it was already too late because he had succeeded in cutting off the two wrists and inflicted a deep cut on my neck,” Idowu narrated her ordeal.
She revealed that street boys who were angry with the incident went after the madman who ran close to a nearby police station where they caught up with him. As the madman was trying to flee again, they set him ablaze because they thought Idowu was dead.
“I was taken to several hospitals to put the severed wrists back to position, but all efforts proved futile due to non-availability of fund. I spent eight months in the hospital before I returned to the village. Good Samaritans later came my way and I was flown to the United States of America (USA) for proper medical attention. I spent five months in America and came back with two artificial limbs,” she recalled.
A lady, in her 30s told The Guardian on condition of anonymity that she was barely nine years old when a mentally deranged man violated her. Her family was helpless and ever since, she has continued to feel the pain, as she has not completely healed from the trauma.
The lady asked, “Who will ever believe that a madman took your virginity? Who will you tell this? Can you even open up to your husband to tell him this truth?”
Nigeria is reported to be grappling with a staggering mental health crisis, as millions of its citizens suffer from various mental disorders. The World Health Organisation (WHO) estimates that a whopping 20 per cent of Nigerians, or around 40 million people, are affected by mental illness.
Although mental health problems are widespread in many African nations, they rarely receive the attention they deserve. And owing to the limited understanding of mental health disorders at the primary health-care level, caring for individuals with mental health issues is often left for family members.
While inadequate facilities stands as a major challenge, a check at the available mental health facilities across the country showed that while a few states can boast of having psychiatric hospitals, majority of the hospitals lack basic amenities.
It was learnt that majority of the facilities are struggling with inadequate bed spaces; outdated equipment; and limited access to medical imaging, resulting in inadequate care and long waiting times for patients.
Mental disorder, also known as mental illness or psychiatric disorder, has a pattern of behavioural, emotional or cognitive symptoms that cause distress that impairs daily functioning, and deviation from cultural norms. Its characteristics include abnormal thoughts, feelings or behaviour, persistent or recurrent symptoms and interference with daily life, relationship, or work.
Investigations and research have shown that the challenges facing the country’s psychiatric care system include shortage of psychiatrists and mental health professionals, poor funding, cultural and religious beliefs, inadequate infrastructure, lack of awareness about mental health issues and multigenerational trauma.
The Guardian investigations show that owing to infrastructure challenge and dearth of professionals, there has been a major hindrance to effective mental service delivery. Investigations show that mental health cases in the country are increasing at an alarming rate.
It was gathered that the funding for mental health care is limited, with only a small fraction of the central government’s health budget (3 to 4 per cent) dedicated to mental health. Of this amount, over 90 per cent goes to a handful of neuropsychiatric hospitals, leaving a few resources for other facilities.
The Medical Director, Federal Neuropsychiatric Hospital, Yaba (FNPHY), Lagos, Dr Olugbenga Owoeye, confirmed that Nigeria has only 10 stand-alone psychiatric hospitals in 10 states, which, according to him, are grossly inadequate “because every state is supposed to have at least one psychiatric hospital.”
According to Owoeye, the Federal Neuropsychiatric Hospital, Yaba is experiencing a drastic swell in the number of fresh cases. This revelation gave credence to the fact that the few psychiatric hospitals in the country are already burdened.
He noted that the hospital has seen a spike from between 150 and 300 monthly to between 750 and 900 currently.
“Before, we used to see, on average, five to 10 new cases of patients breaking down every day. But now, we are seeing 25 to 30 new cases every day, and they are not those people who are coming for check-ups,” the medical director said.
A consultant psychiatrist, Neuropsychiatric Hospital, Aro, Abeokuta, Ogun State, Dr. Emmanuel Abayomi, who also stated that the country is challenged with dearth of psychiatric hospitals, said there are nine stand alone federal psychiatric hospitals, in addition to about 12 federal university teaching hospitals, with in-patient psychiatric services domiciled within their facilities.
He added that there are about 15 state-government run psychiatric facilities across the federation. He added that nearly all state government-run medical school teaching hospitals and privately run university medical school teaching hospitals provide some form of mental health care services.
“In addition to these, there are quite a good number of private mental health care facilities, especially in the urban centres.”
Despite these, experts say the facilities are grossly inadequate to cater for the growing number of patients.
It was learnt that the spike in the number of mental patients and inadequate infrastructure to cater for their treatment is gradually assuming a dangerous dimension in the country, as the number of those roaming the streets, markets, communities and highways are increasing astronomically.
Reports indicate that Nigeria has only 0.5 beds per 1,000 people, far below the World Health Organisation (WHO) recommended four beds per 1,000 people, while over 60 per cent of x-ray equipment is obsolete, as some are dating back 10 to 60 years. The country could boast of only 58 Magnetic Resonance Imaging (MRI) machines as of 2018.
The painful aspect of this development is the growing number of patients besieging these facilities.
As a confirmation of this, the World Health Organisation (WHO) reports that one in seven adolescents suffer from one mental illness or another and the number increases as they move to adults, where one in four adults suffer from one mental illness or another. This further compounded the problems associated with these mental health facilities.
Abayomi, who attested to the rising number of patients, argued that the trend is not peculiar to Nigeria, it is a global situation. He lamented that the sharp rise in mental health care needs of patients, is far beyond the available facilities and trained mental health personnel.
On the growing number of new patients, he said: “This increase happens in two ways. Firstly, the number of persons who newly report having mental health struggles is on the increase. On the other hand, people who have been previously diagnosed with a mental health condition are suffering more relapses by the day.”
The issue of shortage of psychiatrists and mental health professionals seems to have defied all possible solutions, especially with the mass exodus of health officials to foreign countries.
Beyond psychiatrists, there is also a shortage of psychologists in the country. Psychologists are key professionals in providing services for people with mental conditions such as behavioural problems, learning difficulties, depression, and anxiety.
This development has also been aggravated by brain drain, with many mental health professionals leaving the country in search of greener pastures.
Experts claim that aside from funding, the issue of brain drain in the sector is also majorly caused by poor state of infrastructure, driving many mental health professionals to seek better opportunities abroad.
Abayomi, who rued the untoward development, said with the meager number of psychiatrists, a doctor would be catering for over one million patients.
“Nigeria currently has one psychiatrist to cater for the mental health needs of over one million people! And this is precarious, both for the psychiatrist and the country. The psychiatrist is at risk of increased stress and burnout. And don’t forget, the psychiatrist is also a human being, who is equally at risk of mental health struggles.
“Physician burnout among psychiatrists is quite concerning. They may choose to migrate, or quit practice altogether, further depleting their number, and discouraging young doctors from choosing to specialise in psychiatry. For the country, we stand the risk of worsening brain drain on one hand, and poor economic growth on the other hand, as a mentally struggling workforce cannot successfully drive the economic growth that our nation’s leaders are working on.”
On his part, Owoeye said the concern for professionals is due to the growing inability of the care facilities and their workforce to adequately meet the rising demands for mental well-being. He acknowledged the gross inadequacy of mental health experts globally, which is one of the factors promoting the brain drain of health professionals in Third World countries like Nigeria.
The medical director grieved that Nigeria currently has less than 300 psychiatric doctors and even lesser number of occupational therapists, a few number of clinical psychologists, as well as a few psychiatric nurses and social workers.
“That means that there are less than 300 psychiatrists to take care of over 200 million people. Some states do not have a single psychiatrist, while the majority of these numbers are in Lagos, Abuja, Kaduna, Port Harcourt, and Enugu, because we are so small in number, we know ourselves.”
He listed other challenges compounding the inadequate manpower in the country to include high cost of education, long duration of training, as well as inadequate infrastructure.
On the negative effect of this development on the society, Abayomi said: “Sadly, not only is it a fact that we don’t have enough psychiatric facilities and new ones are not being built, the few available trained mental health professionals are either actively relocating abroad in search of greener pastures, or retiring from public service.
“And this has numerous negative on the society. First is the overall health and wellbeing of individuals that constitute the society.As a society is the sum of its individual persons and more, a mentally unwell individual who’s unable to access quality healthcare makes for a mentally unhealthy society. In other words, if the society is sick today, it is perhaps her people are going through mental health struggles, with no sufficient resources to help them.
“Second is the negative impact of this on family health. Undiagnosed and untreated mental health conditions can lead to family conflicts, marital separation and divorce, not to mention intimate partner violence or domestic violence, and the untold harm this does to children raised in such families. Such children may grow up to bear the scars of childhood trauma – leading another gamut of mental health struggles – continuing another cycle of psychiatric disorders.
“A third negative impact is on the workplace and education. Students with mental health struggles who are unable to get treatment may suffer poor grades and failures in school, and eventually withdraw from school. Some persons fail to get advanced degrees because of anxiety disorders for example. And for the employed, patients with schizophrenia, for example, may resign from their jobs without full awareness of their actions, perhaps because they heard a voice telling them to do so.
“Bosses may unknowingly make the work-environment toxic, further exacerbating the already fragile mental health of their staff. And this sometimes spirals out of control. There is a gale of resignations, a high staff turnover, dwindling company finances, mass retrenchment, and eventual company collapse, leading to unemployment and its own attendant mental health risks,” Abayomi said.
He noted that the issue affects the society at large and there is a heightened state of anxiety, low morale, undue suspiciousness and paranoia. “We all feel unsafe in a hostile world. The health and safety of our world rests solidly on how compassionately we care for those among us with mental health struggles.”
A sociologist, Mr. Dokun Gabriel, warned that the development portends great danger to the society.
“Majority of these psychiatric patients act violently, and are very aggressive with uneven emotional temperaments. We have had stories of psychiatric patients attacking people, with records of death, while some are left with permanent injuries.
“The dearth of mental health facilities and shortage of manpower will endanger the lives of Nigerians as these patients will continue to roam the streets, board same bus with sane people and also transact business with others in the same market.”
“It is obvious that one of the major challenges facing the sector is funding. Unlike in the other climes, record shows that budget for this sector is still within three to four per cent yearly. If the budget is improved, it will provide opportunity to build new facilities, improve the welfare of psychiatrists travelling abroad to seek greener pastures and also provide them opportunity to train new officials,” he said.
Gabriel cited the protest by some patients of the Neuropsychiatric Hospital, Aro, Abeokuta last May over alleged poor treatment by the hospital, when one of the doctors was attacked, while the nurses and other doctors took to their heels.
“We learnt that the patients were protesting poor feeding, poor sanitary system, general insensitivity on the part of the management of the hospital, absence of an alternative source of power each time there is a power cut from the Ibadan Electricity Distribution Company, among others.
“There are reports that the entire staff of the health facility were taken by surprise. More of this should be expected if government fails to do the needful, by increasing budget for the sector, provide infrastructure, enhance the welfare of the psychiatrists and provide amenities to make the hospitals comfortable for the patients.”
 On the way forward, Gabriel said Nigeria’s mental health care system requires urgent improvement. “More than a quarter of the Nigerian population has mental health issues. Since legislation alone will not change practices, the improvement of mental health services has to be waged on several fronts. Actual commitment of the Nigerian government will be needed for a correct execution of the legal framework, via the provision of financial, material, and human resources.
On the way forward, Gabriel said Nigeria’s mental health care system requires urgent improvement. “More than a quarter of the Nigerian population has mental health issues. Since legislation alone will not change practices, the improvement of mental health services has to be waged on several fronts. Actual commitment of the Nigerian government will be needed for a correct execution of the legal framework, via the provision of financial, material, and human resources.
“This development is a time-bomb, if not urgently addressed, especially with the current economic reality in the country that has pushed many to the extreme. We may not find it easy to move freely on the streets anyone, if the available facilities are not enough to accommodate the patients.”
Stakeholders in the medical sector, including employers, healthcare providers, and the government should collaborate to integrate mental health care into primary healthcare, establish more mental health training institutions, and increase funding for mental health services.
Experts said integrating mental health into primary healthcare in Nigeria would help improve access to affordable mental health services. According to them, many countries, such as Argentina, Australia, and the United Kingdom, have already recognised the importance of mental health as part of primary care, resulting in better health outcomes.
A research has shown that one way to achieve this in Nigeria is to establish community-based rehabilitation centers in rural areas with strong primary care networks. These centers can provide complementary care and work closely with secondary and tertiary care centres. The centres can also serve as training sites for psychiatric residents, primary care physicians, and nurses.
Scarcity of public education about mental health has led to many myths and misconceptions, and a low public acceptance of people with mental health issues. Besides, cultural and religious preconceptions have substantial impact on the healing process of people with mental health disorders.
In 1916, the country enacted its first mental health legislation, which was called the Lunacy Ordinance. This legal framework was revised in 1958, under the name Lunacy Act, to grant magistrates and medical professionals authority to detain individuals with mental health problems.
In 1991, Nigeria’s first mental health policy was established, and its elements included promotion, advocacy, prevention, treatment, and rehabilitation.
In 2003, the National Assembly of Nigeria received a mental health bill to address the many defects of the 1958 law, which were associated with a misunderstanding of mental health issues and scarcity and ineffectiveness of treatments available at that time. However, the bill was withdrawn in April 2009.
Despite being reintroduced in 2013, the bill was not passed into law owing to lack of support. However, on January 5, 2023, the Nigerian President signed the Mental Health Bill 2021 into law, replacing the outdated 65-year-old Lunacy Act.
Experts noted that without adequate funding, implementing any of the policies enunciated in the Mental Health Act 2021 would be impossible.
According to them, it is crucial for the government to increase the allocation of funds from health budgets to improve the accessibility, quality, and affordability of mental health services in Nigeria. With more resources, it will be possible to establish additional rehabilitation centres and train more mental health professionals, thus improving access to quality care and support for those in need.
Aloysius Odii and NnennaMba-Oduwusi, in their Mental health services are scarce in Nigeria but there’s a huge need: what we learnt from callers to a hotline raised the need for emergency hotlines, saying they have a crucial role to play in improving access to mental health services, particularly in countries where these services are in short supply.
They also raised the need for increased advocacy efforts to encourage people to use the free emergency hotline services.
“Nigeria has not actively pursued installing hotlines to support people in need of mental health support. The idea is relatively new in developing countries, including Nigeria.
“Our research shows that people are open to receiving mental health services outside the formal health facilities. This is a huge plus considering the limited number of mental health facilities and health professionals serving the huge population in need of care. However, we call for studies to evaluate the cost of providing mental health services through hotlines,’’ they said.






