• Public facilities record 750 to 900 new cases monthly
• 1 in 7 adolescents, 1 in 4 adults mentally ill globally
• Nigeria left with about 300 psychiatric doctors, fewer occupational therapists, others
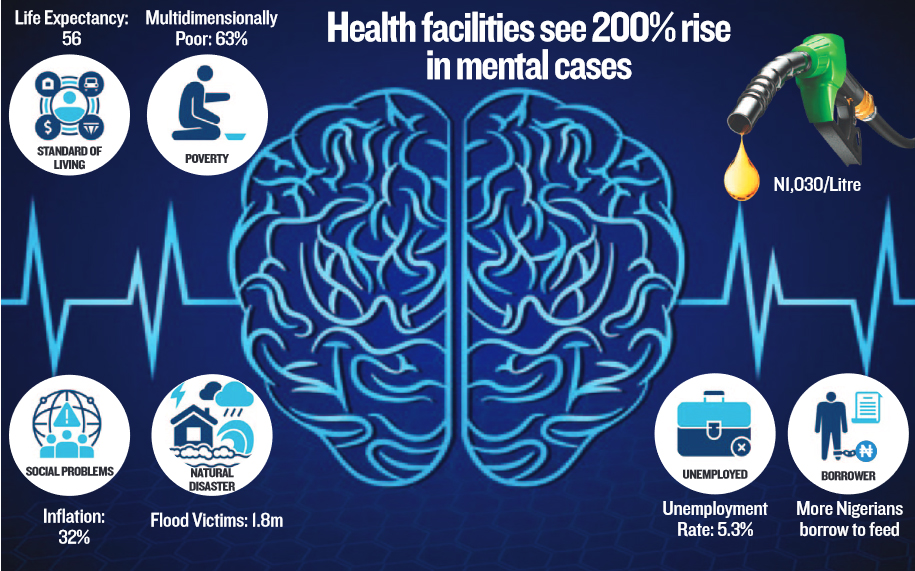
Worsening pangs of life and living in Nigeria are pushing more citizens to the edge, with mental health cases presented in care facilities now 200 per cent more than the previous year’s record.
While the heavy traffic could have meant more attention to mental health, most of the cases presenting at psychiatric hospitals are at the critical end, requiring emergency services than the overwhelmed facilities can afford.
Commemorating World Mental Health Day today, stakeholders emphasised that the socio-economic realities are running adults and adolescents crazy, and in need of urgent interventions across multiple levels.
While the rising cases of anxiety disorders, depression and suicide tendencies are not peculiar to Nigeria, the recent plunge in socioeconomic fortunes is running many people in Nigeria amok.
Following the current administration’s twin policies of fuel subsidy removal and floating of the naira, the cost of living and inflation have peaked across the board. As of August 2024, inflationary pressure was pegged at 32.15 per cent.
With more manufacturers and multinationals unable to bear the cost of operations and closing shops to worsen the already bad unemployment rate of 40 per cent, many breadwinners are despondent coping with the high cost of feeding, shelter, utility bills, health and school fees. Except for the political class, the economy is in dire straits for all.
Mental health expert at Pinnacle Medical Services, Dr Maymunah Kadiri, reckoned that the overall local economic challenges are closely linked to the rise in mental health issues.
The worst is that the current trend is accompanied by an increase in substance use disorders, anxiety and depression. Kadiri said: “Poverty-related stress is a major issue, with families facing housing instability, food insecurity, and inability to afford medical care. Chronic stress leads to more mental health problems like depression and anxiety,” she said.
According to Kadiri, patient intake has surged rapidly. “While the emergency departments report rising cases of suicidal attempts and substance abuse, community-based services are overwhelmed with demand.
“At our centre, Pinnacle Medical Services, we have also noticed an increase since the Covid-19 era. From less than five per cent of adolescents and young people to 25 per cent,” she said.
Painting a more graphic picture, the Medical Director of the Federal Neuropsychiatric Hospital, Yaba (FNPHY), Lagos, Dr Olugbenga Owoeye, told The Guardian that the flagship public facility has lately seen a drastic increase in the number of new cases.
This has spiked from five to 10 patients daily to currently about 25 to 30 patients indicating over a 200 per cent increment with at least 750 new cases received at the hospital monthly.
Owoeye said: “Before, we used to see, on average, five to 10 new cases of patients breaking down every day. But now, we are seeing 25 to 30 new cases every day, and they are not those people who are coming for check-ups.”
The World Health Organisation (WHO) reports that one in seven adolescents suffer from one mental illness or another and the number increases as they move to adults where one in four adults suffer from one mental illness or another.
Yearly commemorated Mental Health Day on October 10, the World Federation for Mental Health (WFMH) alongside WHO, raises awareness, highlighting the importance of mental well-being to change the narrative, counter misconceptions and stigma as well as address issues and challenges hindering the promotion of mental health in different settings of life.
The global campaign for World Mental Health Day (WMHD) 2024 is themed: ‘It is Time to Prioritise Mental Health in the Workplace’ and aimed at promoting and prioritising a safe working environment.
Mental illness is a state of psychological disturbance in the memory, emotion, thinking, and behaviour, which becomes so severe enough to cause pain or distress to the person concerned or those who are living around him/her, causing impairment in the social and operational functioning of the concerned.
Owoeye explained that psychological disturbance often gets so serious enough to cause pain or distress, more often not to the sick person but to the people around them.
“In the house, s/he (the sick) will not be able to relate (well) with the wife, husband or children. He will not sleep nor allow others to sleep and everyone will be a suspect in the working place. And then s/he becomes a nuisance on the streets and as a result, the relatives will be feeling the shame which is painful to them,” he said.
The Medical Directors added that the worry for professionals is the growing inability of the care facilities and their workforce to adequately meet the rising demands for mental well-being. Owoeye acknowledged the gross inadequacy of mental health experts globally, which is one of the factors promoting the brain drain of health professionals in
Third World countries like Nigeria. He lamented that Nigeria currently has less than 300 psychiatric doctors and an even lesser number of occupational therapists, very little number of clinical psychologists as well as few psychiatric nurses and social workers.
“That means that there are less than 300 psychiatrists to take care of over 200 million people. Some states do not have a single psychiatrist, while the majority of this number are in Lagos, Abuja, Kaduna, Port Harcourt, and Enugu. Because we are so small in number, we now know ourselves,” Owoeye said.
Other challenges compounding the inadequate manpower in the country according to him include the high cost of education, long duration of training as well as inadequate infrastructure.
“We have only 10 stand-alone psychiatrist hospitals in 10 states, which is grossly inadequate because every state is supposed to have at least one psychiatric hospital,” he said.
On how to improve mental health care amid the odds, clinical psychologists called for an increase in awareness campaigns.A clinical psychologist, Dr Miracle Ihuoma, said given that most mental illnesses have their triggers in the economic realities, awareness should be created within family structures to empower parents on mental health to help prepare their children on how to deal with the challenges that come with adulthood.
Speaking on the theme of this year’s WMHD, Ihuoma pointed out that mental health and work are interconnected in such a way that when one gets affected, it equally affects the other. He continued that conversations about mental health within the work environment should be promoted through employer-centred programmes and encouraged organisations to make provisions for psychological health packages just like fiscal health packages for employees.
Another clinical psychologist, Alawode Yussuff, advocated early education and sensitisation to improve prevention, which is much cheaper than treating the illness.
“Catching and educating them young is much cheaper than treating the illness. There are lots of childhood depression and anxiety that are unnoticeable, which students in primary school go through daily like being bullied by their classmates, and their friends, and being talked down on. Yes, they get home as well,” he said.
According to him, calling for the promotion of an inclusive environment will empower people to speak up more and reduce stigmatisation. Annually, more than 720,000 people die by suicide globally with 73 per cent of this number taking place in low-and-middle-income countries according to WHO, making suicide the third leading cause of death among 15 to 29-year-olds.
In Nigeria, the Association of Psychiatrists in Nigeria (APN) has called for the decriminalisation of suicide to encourage open suicide discussions, promote preventive measures as well and protect the rights and privileges of families under the burden of suicide.
A professor of psychiatry, Taiwo Latif Sheikh said Nigeria is within a high suicide terrain which has reached a crisis point that not only threatens our existence but also the future of young Nigerians. He noted that over two-thirds of global suicide takes place in low-middle-income countries while the current estimated suicide rate in Nigeria is about 6.9 per 100,000 population, indicating about 15,000 deaths by suicide yearly.
“For every single death that we record as a result of suicide, there were about 20 to 25 attempts and for every suicide, a minimum of six people within the family setting will suffer one psychosocial disturbance either depression or anxiety or some other mental health condition so by the time you are multiplying this you realise that about 300,000 people will suffer one mental health condition or the another as a result of suicide that 15,000 people have committed in Nigeria,” he lamented.
Sheikh who is also on the advisory board of the Africa Centre for Disease Control explained that the Nigerian law currently criminalises suicide and punishes suicide attempts making it difficult for people to discuss issues of suicide openly which is a first step towards suicide prevention and intervention.
According to Sheikh, Nigeria is at the headquarters where factors that lead to suicide are over-represented among young people with about 85 per cent moving around with untreated mental health conditions due to inaccessibility or affordability of the right care.






