In Greek mythology, Pandora’s box was opened and every manner of ills was unleashed on mankind. By the time it was shut only hope was left in the jar, in today’s pandemic world, the Pandora’s box is being shut against chloroquine, the immediate hope in these present times. In Homer’s Iliad, chloroquine would have been in the good urn while the novel coronavirus would be in the evil urn.
Coronaviruses are respiratory viruses. Hundreds of coronaviruses exist but only seven have been known to affect humans. Four of these viruses cause influenza with mild symptoms of common cold and diarrhoea. These four viruses are named human coronavirus HCoV-229E, HCoV-OC43, HCoV-NL63 and HCoV-HKU1. Out of these four, two were identified in the mid-1960’s. These were human coronavirus 229E and human coronavirus OC43. Human coronavirus 229E was isolated in the University of Chicago from a medical student with a cold and human coronavirus OC43 was identified by scientists from the National Institute and Infectious Diseases. The remaining two were identified in Netherlands and in Hong-Kong. These were NL63 isolated in 2004 from a child with pneumonia and HKU1 isolated in 2005 from two other patients with pneumonia. No country or organization thought of making a vaccine against any of these four human coronaviruses then because the symptoms presented were non- life threatening and there was not much research interest in them. Over our lifetimes, we would have had at least one of these four mild viruses that cause the common cold and are usually able to recover without any adverse effects.
Apart from the four human coronaviruses that are usually considered harmless, the remaining three of the seven known human coronaviruses cause more significant infections including epidemics. They are SARS-CoV, MERS-CoV and SARS-CoV-2. The first of these is the SARS-CoV which causes Severe Acute Respiratory Syndrome (SARS) and is different from SARS CoV-2 which causes COVID-19. The virus that causes (SARS) SARS-CoV is sometimes written as SARS-CoV-1. These three coronaviruses cause severe lower respiratory tract infection and infected persons can progress to develop Acute Respiratory Distress Syndrome (ARDS) and multiple organ failure.
The human coronaviruses can also be sub-grouped into alpha and beta. The reservoirs of the human coronaviruses are bats and rodents. The beta human coronaviruses include the coronaviruses that cause epidemics and pandemics; SARS-CoV, MERS-CoV and SARS-CoV-2. Before SARS-CoV first appeared in China, the human coronaviruses were known to cause self-limiting symptoms of the common cold and generally thought to be harmless.
The SARS-CoV was first reported in humans in Southern China in November, 2002 and was responsible for 774 deaths and 8000 infections across 26 countries between 2002 and 2003. It causes a severe viral pneumonia and killed approximately 10 percent of the infected persons giving a high case fatality rate, higher than COVID-19. Transmission is from person to person contact with respiratory secretions. Persons infected with SARS-CoV quickly display symptoms allowing infected persons to quickly isolate and thereby limit the spread of the disease. Only one country in Africa had a case of SARS-CoV and that was South Africa.
The Middle East Respiratory Syndrome (MERS) was first reported in September 2012 and first identified in Saudi Arabia. Camels are a reservoir of MERS. Transmission is usually by contact with an infected animal. Person to person transmission by close contact is also possible. To date, 27 countries have had cases of MERS. There have been about 2400 cases and 858 deaths due to MERS. The MERS has killed about 35 percent of the infected persons giving a case fatality much higher than SARS.
The SARS-CoV-2 first appeared in humans in December 2019. It was unofficially called the Wuhan virus because it was first reported from the city of Wuhan in China. Later it was tentatively named 2019 novel coronavirus (2019-nCoV). On the 11th of February, the novel coronavirus was officially named by The International Committee on Taxonomy of Viruses (ICTV) as “Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)”. The disease was named coronavirus (COVID-19). The 19 is signifying the year it was first reported in humans. The SARS in the name, SARS-CoV-2 was chosen because of its genetic cousin in the SARS outbreak that occurred between 2002 and 2003 in Asia. The virus responsible for the 2002-2003 Asian outbreak; SARS-CoV should not be confused with today’s SARS-CoV-2.
Globally, by the 24th of August, there were over 23 million (23, 647,429) cases of COVID-19. Sixteen million people had recovered (16,137,412). The case fatality is 3.4 percent, lower than the fatality from SARS-CoV of 2003 but more infectious. The case fatality for COVID-19 was higher in the months of March and April. Those infected with SARS-CoV-2 can shed the virus in the first week of infection and not show symptoms of infection allowing the virus to spread quickly. About one-quarter of people infected with SARS-CoV-2 are asymptomatic.
Approximately eight hundred thousand persons (813,578) have died from the disease and it has spread to at least 188 countries. A handful of countries, about twelve countries mainly from the Polynesian islands have not reported any case of COVID-19. Although it is geographically close to China, North Korea has also not reported any case of COVID-19. Being one of the most reclusive countries, it is doubtful it has not seen any case of COVID-19.
To date there is no cure or vaccine for any of the human coronaviruses. The treatment is usually supportive. However, like the hope crying out of Pandora’s box, chloroquine is still the only immediate hope in the management of COVID-19. Pairing of aggressive testing with massive contact tracing of all populations exposed is another hope but not economically and socially accessible for most countries especially African countries. Only few countries have achieved massive and aggressive mass testing with contact tracing. By the 24th of August, Nigeria had only tested 383,130 persons.
South Korea with a population of 51 million engaged in massive testing paired with equally massive contact tracing. Despite South Korea’s close proximity to China, by the 24th of August, South Korea had a case fatality of 309 persons, 17,665 confirmed cases and had tested over 1.8 million people. At the peak of the pandemic on the 9th of April, South Korea had tested 494,711 people, had 10,423 cases and recorded 204 deaths. It had a case fatality of 1.95 percent. The global case fatality in April was 4.34 percent.
Taiwan, considered a breakaway province from China had the highest mortality rate in the world during the 2002-2003 SARS outbreak and has learnt many lessons in managing COVID-19. By the 25th of August, Taiwan had only 487 cases, 462 recovered cases and 7 deaths. The case fatality was 1.43 percent in a population of 23.78 million. It has conducted tests on 173,081 persons. The case fatality on 26th of August was 3.43 percent.
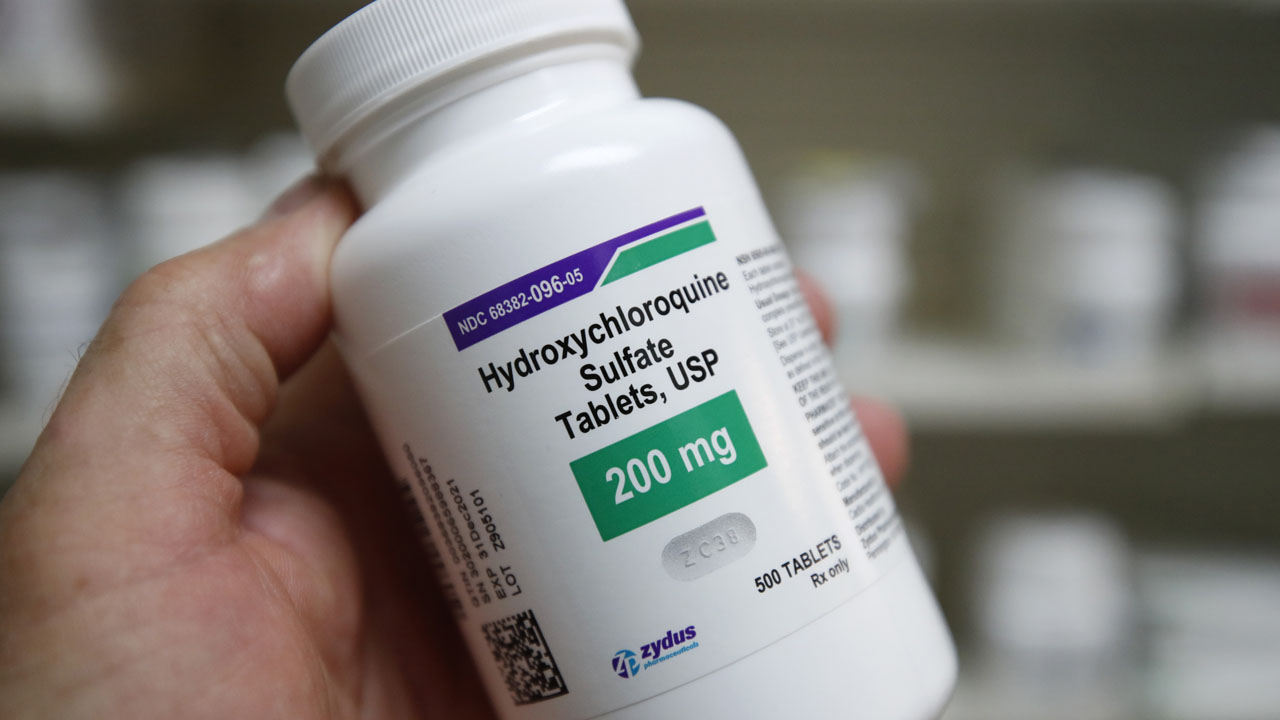
Vaccine is a future hope in the management of COVID-19. Therefore, for the moment an immediate hope in the management is chloroquine and its sibling hydroxychloroquine. Chloroquine is a known drug, that has been used by humans for more than ninety years and is inexpensive. It was first synthesized in 1934 by a German pharmaceutical company. Quinine is a precursor of chloroquine. Quinine is a naturally occurring compound that can be found in the bark of Cinchona trees. Before the advent of chloroquine, quinine was used in the treatment of malaria. Hundreds of years before the colonization of Africa, our forefathers used herbal remedies in the treatment of malaria.
In Nigeria we have many other plants that are used in the treatment of malaria. These plants possess antimalarial properties attributed to anthraquinones and anthranquinols. Quinones and quinols are different from quinine but they are all antimalarials. Derivatives of quinine and artemisinin are the two main sources of modern antimalarial drugs. Artemisinin is derived from a Chinese plant known as sweet wormwood.
Today, herbal remedies are still being used all over Nigeria because they are easily accessible and the consumers have trust in them. There are over 1200 plant species from more than 160 plant families that have been successfully used in the treatment of malaria. Some of the popular herbal preparations are Dongoyaro/Neem (Azadirachta indica A. Juss), Bitter Leaf (Vernonia anygdalina Del.), Mango (Mangifera indica L.) and Citrus Fruit (Citrus medica). These remedies are usually made from the fruit, bark, stem or leaves of the plant and consumed as a drink, steam-inhaled and used as a bathing water for 4-10 days or until symptoms subside. In some households, they are consumed daily as a prophylactic. The continuous consumption of these herbs for prolonged periods can cause damage to the liver and kidneys.
Therefore, the use of chloroquine in known dosage preparations for the treatment of malaria is a welcome relief from the infrequent liver and kidney damages caused by some of these herbal preparations.
Obilade, a medical doctor and an Associate professor of Public Health, wrote from Abuja.






